
PODIUM. Journal of Science and Technology in Physical Culture, January-April; 16(1): 248-261
Translated from the original in spanish
Practical evaluation of a physical-therapeutic exercise program in patients with amyotrophic lateral sclerosis
Valoración práctica de un programa de ejercicios físico-terapéuticos en pacientes con esclerosis lateral amiotrófica
Avaliação prática de um programa de exercícios físico-terapêuticos em doentes com esclerose lateral amiotrófica
Yordán Cañadilla
Barrios1![]() https://orcid.org/0000-0002-2835-3559
https://orcid.org/0000-0002-2835-3559
Magda Mesa Anoceto2![]() https://orcid.org/0000-0002-7216-0121
https://orcid.org/0000-0002-7216-0121
Jerry Bosque Jiménez2![]() https://orcid.org/0000-0001-5978-8187
https://orcid.org/0000-0001-5978-8187
Rodolfo Ruvenio Vidaurreta Bueno2![]() https://orcid.org/0000-0001-6942-1047
https://orcid.org/0000-0001-6942-1047
Annia Caridad Cañete Rojas1![]() https://orcid.org/0000-0001-5757-6973
https://orcid.org/0000-0001-5757-6973
1Institute of Neurology and Neurosurgery. Havana, Cuba.
2University of Physical Culture and Sports Sciences "Manuel Fajardo". Havana, Cuba.
*Corresponding author: yordanreh@gmail.com
Received:25/10/2020.
Approved:12/01/2021.
ABSTRACT
Given the need to design specific intervention strategies for patients with Amyotrophic Lateral Sclerosis (ALS), incorporating Rehabilitation and Physical Culture contents from an integrative perspective, a physical-therapeutic exercise program was developed specifically for these patients at the Institute of Neurology and Neurosurgery, to contribute to slow the progression of the disease, attenuating symptoms, signs and complications. The aim of the study was to evaluate in practice the efficacy of the physical-therapeutic exercise program applied. A longitudinal study was conducted and used the pre-experiment of samples related to patients diagnosed with ALS in the period 2014-2019, evaluating the results of the first three months of application, with follow-up planned after these. In the processing of the recorded data, the empirical distribution of frequencies and their graphical representations; descriptive measures (arithmetic mean and standard deviation); binomial test; test 2 for two independent samples, applied to contingency tables; Student's t-test for related samples, and Shapiro Wilks test were used. As a result, 71.05 % of the patients included in the study presented a plateau in the behavior of their clinical picture, which corroborates the benefits of the program and its effectiveness, through the use of physical-therapeutic exercises, respiratory and nutritional support, contributing to the delay of the progression of the disease from one stage to the other of the functional classification.
Keywords: Physical-therapeutic exercises; Rehabilitation; Amyotrophic lateral sclerosis.
RESUMEN
Dada la necesidad de diseñar estrategias de intervención específicas para pacientes con Esclerosis Lateral Amiotrófica (ELA), incorporando contenidos de Rehabilitación y Cultura Física desde una perspectiva integradora, se conformó un programa de ejercicios físico-terapéuticos, específico para estos pacientes en el Instituto de Neurología y Neurocirugía, para contribuir a retardar la progresión de la enfermedad, atenuando síntomas, signos y complicaciones. El objetivo del estudio consistió en valorar en la práctica la eficacia del programa de ejercicios físico-terapéuticos aplicado. Se realizó un estudio longitudinal y se utilizó el pre-experimento de muestras relacionadas a pacientes diagnosticados de ELA en el periodo 20142019, evaluándose los resultados de los tres primeros meses de aplicación, con seguimiento previsto posterior a estos. En el procesamiento de los datos registrados, se utilizó la distribución empírica de frecuencias y sus representaciones gráficas; medidas descriptivas (media aritmética y desviación estándar); la prueba binomial; la prueba c2 para dos muestras independientes, aplicada a tablas de contingencia; la prueba t de Student para muestras relacionadas, y la prueba Shapiro Wilks. Como resultado de ello, el 71,05 % de los pacientes incluidos en el estudio presentaron una meseta en el comportamiento de su cuadro clínico, lo que corrobora los beneficios del programa y su eficacia, mediante el empleo de ejercicios físico-terapéuticos, respiratorios y apoyo nutricional, contribuyendo al retardo de la progresión de la enfermedad de una etapa a la otra de la clasificación funcional.
Palabras clave: Ejercicios físico-terapéuticos; Rrehabilitación; Esclerosis lateral amiotrófica.
RESUMO
Dada a necessidade de conceber estratégias de intervenção específicas para pacientes com Esclerose Lateral Amiotrófica (ELA), incorporando conteúdos de Reabilitação e Cultura Física numa perspectiva integradora, foi desenvolvido um programa de exercício físico-terapêutico especificamente para estes pacientes no Instituto de Neurologia e Neurocirurgia, para contribuir para retardar a progressão da doença, atenuando sintomas, sinais e complicações. O objetivo do estudo era avaliar na prática a eficácia do programa de exercício físico-terapêutico aplicado. Foi realizado um estudo longitudinal e utilizado o pré-experimento de amostras relacionadas com pacientes diagnosticados com ELA no período 2014-2019, avaliando os resultados dos primeiros três meses de aplicação, com acompanhamento planeado após estes. No processamento dos dados registados, foram utilizadas a distribuição empírica das frequências e as suas representações gráficas; medidas descritivas (média aritmética e desvio padrão); o teste binomial; o teste c2 para duas amostras independentes, aplicado a tabelas de contingência; o teste t de Student para amostras relacionadas, e o teste de Shapiro Wilks. Como resultado, 71,05 % dos pacientes incluídos no estudo apresentaram um patamar no comportamento do seu quadro clínico, o que corrobora os benefícios do programa e a sua eficácia, através do uso de exercícios físico-terapêuticos, apoio respiratório e nutricional, contribuindo para o atraso da progressão da doença de uma fase para a outra da classificação funcional.
Palavras chave: Exercícios físico-terapêuticos; Reabilitação; Esclerose lateral amiotrófica.
INTRODUCTION
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disease characterized by progressive muscle paralysis that reflects a degeneration of motor neurons in the central nervous system (upper motor neurons) and, specifically, in the primary motor cortex, corticospinal tract, brainstem and spinal cord (lower motor neurons). In this pathology, there is a paralysis of voluntary muscles that spreads from an initial point of involvement to adjacent regions, and continuously and progressively affects mobility, speech, swallowing or breathing; however, ocular mobility, skin sensitivity, sphincter control and mental functions remain intact in most cases (Barrera et al., 2017).
Traditionally, symptomatic treatments for patients diagnosed with ALS have been planned by physicians specialized in Neurology, Physical Medicine and Rehabilitation, supported by physiotherapy techniques and methods, as well as the use of physical therapeutic agents. In recent years, discrete changes have been achieved in the increase of survival and quality of life of ALS patients; a result that has been directly related to the systematization of care procedures for these patients. Some drugs such as riluzole and medical procedures, are found in the report for ALS by López-Casero et al., (2019).
Symptomatic management constitutes the best therapeutic alternative to accompany patients, family members and caregivers throughout the care process. On the other hand, no consensus has been established regarding the use or not of physical exercise, its dosage and the response of each patient, in the struggle to slow down the degenerative process of the disease, which makes it a controversial point. Some specialists, such as Johnson & Braddom (1971), do not recommend any resistance or aerobic exercise program, for fear of causing damage by exhaustion. They agreed that very repetitive or heavy resistance exercise can cause loss of muscle strength in the already weakened muscle.
On the other hand, Paganoni, et al., (2015); Plowman et al., 2016 propose that physical-therapeutic exercise under appropriate prescription can be physiologically and psychologically beneficial for those affected by ALS, especially when implemented in the early stages of the disease. Other authors such as: Aldana et al., (2012); Roche et al., (2012); Orridge et al., (2013); Al-Chalabi et al., (2016); Díaz and Ortiz (2017), recommend stages or stages to collect information related to the clinical situation of each patient and define therapeutic intervention alternatives, as well as to establish differences related to symptomatology.
Specifically, it is taken into account Dal Bello-Haas (2018) and Jones et al., (2019), who report in relation to the evaluation of rehabilitation programs, that studies with ALS patients have been conducted with sample sizes too small to pinpoint the extent to which exercise is beneficial or detrimental. They further point out that current practice guidelines for physical therapy management rely heavily on the opinion and consensus of the experts involved in each study. They conclude that more research is needed to define the type of exercise to be performed and the dosage of workloads in specialized care, given the clinical and symptomatological diversity of patients.
In the Institute of Neurology and Neurosurgery (INN) of Cuba, since 2005, a multidisciplinary consultation was created to follow up patients with clinical suspicion of ALS, in order to create a registry and study its frequency, a study based on mortality records and resulted in 0.8 /100000 inhabitants for the whole country (Zaldivar, et al., 2009). In 2013, the Physical Medicine and Rehabilitation Service of the INN began to treat patients diagnosed with ALS, using some physiotherapy techniques (mobilization and some respiratory exercises), use of physical therapeutic agents, and the use of physical therapy.
Thus, scientific concerns related to the treatment itself arise, and some studies are undertaken to select and evaluate the response of patients according to the use of physical-therapeutic exercises and other therapeutic components. This becomes the need to create specific intervention strategies for patients with ALS, incorporating contents of Rehabilitation and prophylactic and therapeutic Physical Culture, as specialties in rehabilitation, from an integrative perspective (Cañadilla, Aguilera, Cañete and Aguilar, 2019).
The aforementioned bases this research and reveals the lack of a methodological approach with specificity for the physical rehabilitation of patients with ALS that would contribute to slow its progression. Therefore, a physical-therapeutic exercise program is designed for the rehabilitation of these patients at the INN.
The course of the research is guided by the following hypothesis: the application of a physical-therapeutic exercise program for the rehabilitation of ALS patients that integrates exercises with specificity in their ordering, sequencing and interrelation according to their location in the functional classification, will contribute to the delay in the progression of the disease.
The objective of the research is to evaluate the efficacy of the physical-therapeutic exercise program for the rehabilitation of ALS patients.
MATERIAL AND METHODS
The study according to its approach was of an explanatory type, which in most classifications is also called experimental research and among these, it is classified as a pre-experimental research, of related samples, where the subjects were their own controls.
It is a longitudinal study where the results shown are those obtained in the first three months of application, with follow-up planned after these three months.
The population consisted of 54 patients diagnosed with ALS by the Multidisciplinary Group of the INN, in the period from 2014-2019, and the sample consisted of 38 individuals selected through non-probability purposive sampling.
Inclusion criteria: patients with a confirmed diagnosis of ALS who met the criteria of Escorial (1994), Arlie House (1998) and Awaji (2006), cited in Galán, López and Matías-Guiu (2015).
Exclusion criteria: patients with decompensated comorbidities.
Output criteria:
a) Poor cooperation or lack of motivation for treatment.
b) Death or voluntary death of the patient.
Ethical considerations: we basically start from what is stipulated in the Nuremberg Code of 1947 and the Declaration of Helsinki 2013, cited in Barrios, Anido and Morera (2016) and request prior informed consent to participate in the study.
The initial state of the phenomenon or fact under research was ascertained, which is identified with the first phase of the program, which is the classification of the ALS patient in one of the four stages established by the program in order to precisely match the exercise program, adjusting to the patient's tolerance and degree of physical deterioration.
The patients included in the study underwent the physical-therapeutic exercise program designed and at the end of three months, an evaluation of the results was made in terms of the delay in the progression from one classification stage to the other of the disease.
The results provided an evaluation of the impact of rehabilitation on the patient's functioning.
Statistical methods were used to process the recorded data such as empirical frequency distributions and their graphical representations; descriptive measures (arithmetic mean and standard deviation); the binomial test; the 2 test for two independent samples applied to contingency tables; the Student's t-test for related samples after checking the normality of the before and after differences by means of the Shapiro Wilks test; the use of a binary logistic correlation matrix in order to express them in the form of a normality test; Student's t-test for related samples after verifying the normality of the before and after differences by means of the Shapiro Wilks test; the use of a binary logistic correlation matrix with the purpose of expressing in the form of probabilities and through the Wald statistic the effect of the set of exercises of the facial musculature, therapeutic, respiratory and nutritional status. In all cases a significance level (alpha á) of 0.05 was set, which corresponds to a rejection zone associated with the probability value p (p < 0.05).
Statistical processing was performed using SPSS version 21.0 for Windows.
The physical-therapeutic exercise program applied follows the following structure: rationale, objectives and content. The content covers the phases of the program and its methodological actions (Phase I. Classification of the patient diagnosed with ALS; Phase II. Programming of the exercises according to the classification of the patient diagnosed with ALS; Phase III. Execution of the program; Phase IV. Control and evaluation) and general methodological indications. The design of this program was favorably evaluated by the Multidisciplinary Group for the care of patients with neurodegenerative diseases of the INN, which is considered an expert. The group evaluated the formal and intrinsic quality of the program, the adaptation and suitability to the context where it is directed and the acceptance of the proposal in that context.
RESULTAS AND DISCUSSION
The study group was characterized by a significant predominance of male sex (Z = 3.2717 p = 0.0011), an average age of 46 years, distributed by age groups (30-39, 40-49, 50-59, 60 and over) where the group of 40-49 years reached the highest frequency. The most frequent personal and family pathological history was arterial hypertension (AHT). The disease was mostly sporadic, only two patients out of 38 had familial ALS and the clinical spinal form predominated.
The most frequent symptoms of the disease at onset were: weakness in the lower and upper limbs manifested in more than 76 % of the cases; language disorders such as dysarthria were present in more than half of those studied (64.8 %) and anarthria in slightly less than half (48.1 %); dysphagia as an initial swallowing disorder was manifested in 57.4 % of the cases; dysphagia as an initial swallowing disorder was manifested in 57.4 % of the cases.
According to the functional classification of ALS patients at the NSB, the 38 patients were placed in one of the four evolutionary stages of the disease by the Multidisciplinary Group of the NSB. They were classified as follows:
It can be seen that most of the patients participating in the study are located in stage II and III, since they arrive at the consultation when they have begun to present clinical manifestations of the disease.
Table 1 shows the results of therapeutic exercises and respiratory exercises according to the evolutionary stages of the disease, in terms of delaying the progression from one stage to the other (Table 1).
Table 1. - Evolution of patients three months after application of therapeutic and respiratory exercises
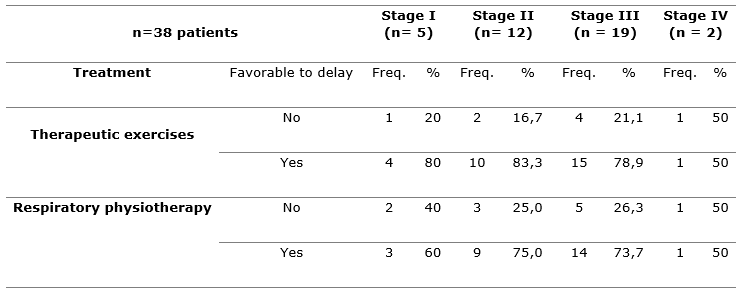
It is observed that in stage I, four and three patients, respectively, evolve favorably in terms of retarding progression; in stage II, 10 and 9; in stage III, 15 and 14; and in stage IV, 1 and 1 patient.
The significance of the proportions (or frequencies) that were observed in the sample was calculated using the binomial test and resulted in p=0.0031 for respiratory physiotherapy and p=0.0003 for therapeutic exercises. The effect of respiratory physiotherapy was very significant according to the probability obtained and so was, even more significantly, the effect of the physical-therapeutic exercises.
The evolution of the patients three months after the intervention with the facial musculature, respiratory and therapeutic exercises is illustrated in Figure 1 (Figure 1).
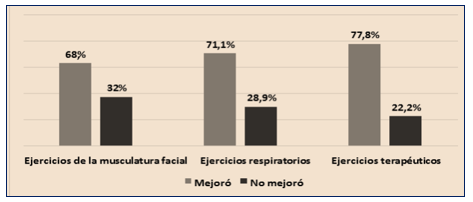
Fig. 1. Results of the evolution of the different types of exercises
The percentages of patients improved with facial muscle exercises, respiratory exercises and therapeutic exercises exceed 50%. The effect of the physical-therapeutic exercise continues to stand out. The overall improvement was at the expense of the physical-therapeutic exercises.
Pulse oximetry was performed in these patients before and after the intervention. Oxygen saturation levels improved in 27 patients. Ten patients did not improve, but developed respiratory compensation mechanisms with values between 88 and 90 %, lower than those obtained before the intervention. In addition, one person in stage IV progressed (death of the patient).
Compliance with the program's indication to keep a record of general data and data of interest to the study for follow-up and control, allowed the review of the files with the purpose of summarizing data related to the impact of the proposal. A total of 36 patients in the study (94.7 %) reported that rehabilitation was benefiting them as it offered relief from different symptoms, helping them to expel secretions, breathe better and reduce muscle pain, among others. They understand that physical exercise helps them to cope with the disease in a positive way, contributes to remain active, helps to correct postural alterations and to reduce muscle stiffness.
A total of 21 patients (55.2 %) reported that the improvement in activities of daily living such as: writing, preparing meals, walking, going up and down stairs, lying down and tucking themselves in, among others, was not significant. On the other hand, 13 (34.21 %) stated that they felt better than before starting the program, and were able to complete some tasks in which they felt exhausted before. Others stated that they were able to reeducate their gait to maintain functional independence and trained in case of falls.
The opinion of 43 family members and caregivers out of 59 registered (72.88 %) was that they observed some improvement in the mental state of the patients and also stated that from the physical and psychological point of view it favored them to face the disease. The relatives of patients in final stages (III and IV) appreciated the participation in the program given the attention given to helping the patient to live the last phase of life with quality, respecting their personal goals and values.
In general, the patients included in the study considered that there are few physical benefits that can be perceived, but it constitutes the best option so far, they appreciated the dedication to each patient, as well as the training to all those involved to face the disease. The 38 patients included in the program agreed to continue with it and 35 (89.4 %) recognized the moment of treatment as the most important in their daily routine.
Compliance with another indication of the program in relation to establishing an effective link with the Nutritional Care Group for Neurological Diseases, in charge of evaluating the patient's nutritional status and achieving adequate nutritional management through recommendations for family members and caregivers aimed at enhancing the response to physical-therapeutic exercises and avoiding the negative consequences of malnutrition, allowed the assessment of the nutritional status of the study sample (Table 2).
Table 2. - Assessment of the nutritional status of the study sample
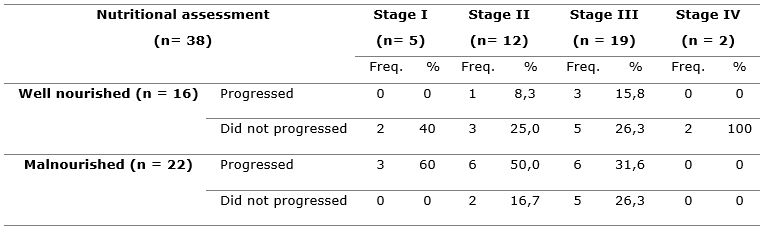
c2 =23,3342 p = 0,0021
In the sample, 16 patients maintained good nutritional status and 22 had nutritional deficiencies. The proportion of well-nourished patients who did not present disease progression was significant with respect to the proportion of malnourished patients.
Of the 16 patients with good nutrition, 12 (75 %) had arm circumference measurements equal to or greater than three centimeters and only four (25 %) less than the initial measurement. On the other hand, in most of them with poor nutrition, 17 (77.3 %), the arm circumference measurement was less than three centimeters and only five patients (22.7 %) increased arm circumference. The relationship between nutritional status and arm circumference was corroborated (2 =14.5518; p = 0.0001< 0.05); well-nourished ALS patients vary with exercise their arm circumference by 3 or more centimeters, more frequently than malnourished ALS patients.
In order to follow over time the response to physical therapy in relation to muscle area, the arm circumference at baseline and at 3 months was compared with that at 3 months (Table 3).
Table 3. - Comparison of arm circumference
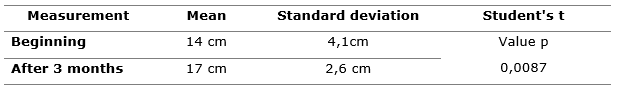
Arm circumference showed an increase in the mean and a decrease in the variability at three months, and it was statistically proven that the changes were highly significant.
Muscle strength behaved as follows: of the patients with good nutrition only two (12.5 %) decreased muscle strength. On the other hand, in patients with poor nutrition 15 (68.2 %) decreased muscle strength. The relationship between nutritional status and muscle strength was corroborated (2 =17.8183;p = 0.0000); well-nourished patients increased their muscle strength with exercise more frequently than malnourished patients.
It was found that the effect of therapeutic exercises, respiratory exercises, facial muscle exercises and nutritional status separately was positive in terms of slowing the progression of the disease, but when combined, it was superior. The values of the Wald statistic confirmed this assertion. The value greater than 4, obtained for the combination, meant that the effect in slowing disease progression from one stage to another was four times more probable than the individual effect. This demonstrates the interaction that exists between the different aspects of treatment and the need for integral and personalized attention, in the sense that the program must be adapted to the characteristics of each case and stage of the disease through which it passes, taking into account variables predictive of survival (nutritional status, ventilatory capacity and muscular strength).
Most of the patients who underwent the application of the physical-therapeutic exercise program and who presented, at that time, good nutritional status, improved significantly in relation to the malnourished patients. The implementation of physical-therapeutic exercises improved their quality of life and functional activity.
This result agrees with the study conducted by Paganoni et al., (2015), who state that nutrition is a predictor of survival and quality of life in ALS patients. They also agree with those obtained by Desport et al., (2010), who obtain that all the parameters evaluated in the follow-up of ALS patients improved after physiotherapy, but significantly in those who presented a good nutritional status.
The results of patient classification at baseline and three months after program implementation are shown below (Table 4).
Table 4. - Functional classification of ALS patients studied three months after program implementation
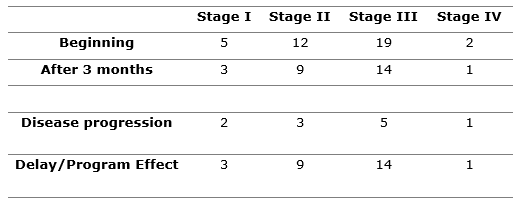
Z= - 2, 433 p=0,0031
There was a plateau phase in the behavior of their clinical picture in 27 of the 38 patients in the study (71.05 %) including patients classified in the four stages of the disease. This proportion was significant according to binomial test results. The results indicate that the benefits of rehabilitation were manifested in all stages of the disease. The patient was kept in the best possible physical condition and his quality of life was improved.
After three months of implementation, the effects of the program were evaluated. The following effects were observed: a plateau phase was established at each stage of the disease; dexterity was optimized by performing a certain movement pattern with less energy expenditure; the movement pattern was modified by performing activities of daily living with greater economy of effort; patients and family members were accompanied to mitigate the negative consequences of signs, symptoms and complications that occurred in the evolutionary process of the disease; support and guidance was provided to the family to participate in the rehabilitation activities; patients and their families learned how to make the most of what they can do at each stage of the disease; physical and psychological problems that could limit success in rehabilitation were addressed, as the program coexisted in the multidisciplinary team.
The results of the program confirmed the criterion that rehabilitation should be offered to all those who suffer some form of disability, not only to those who are expected to recover. Supportive rehabilitation and palliative rehabilitation are established according to the classification given by Tookman, Hopkins and Scharpen (2005). We further concur with Al-Chalabi et al., (2016), in proposing a classification, where current classification systems are combined with the clinical presentation of ALS, imbricating four mandatory components such as: stage of disease, phenotype, diagnosis, and the category according to Escorial criteria, as well as diagnostic modifiers and optional terms, as needed.
Although there are different criteria regarding the use or not of physical exercise, in the struggle to slow the degenerative process of the disease, Paganoni et al., (2015) bet on therapeutic physical exercise, as long as it is prescribed appropriately, in the same way in a study by Luneta et al., (2016), which reports on the possible protective effect that physiotherapy has on ALS patients, superior to usual care without physical exercise.
The evaluation of the physical-therapeutic exercise program confirmed, three months after its application, that the hypothesis that it contributes to the delay of the progression of the disease from one stage to the other of the functional classification is not rejectable. It is important to point out that the results presented above are reached in a particular context, in a sample not uniformly distributed by stages of functional classification of the disease, with an evolutionary follow-up time of three months, aspects which determine the limits of the research.
CONCLUSSIONS
The evaluation of the program corroborates its effectiveness, understood as the way in which it responds to the expected results (facilitating compliance with the objective of focusing on what the patient needs most at a given time in the course of the disease, to maintain maximum function and quality of life, and contributing to slowing the progression of the disease from one stage to the next in the functional classification) by using the necessary means (physical-therapeutic and respiratory exercises and nutritional support).
REFERENCES
Al-Chalabi, A., Hardiman, O., Kiernan, M. C., Chiò, A., Rix-Brooks, B., & Berg, L. H. van den. (2016). Amyotrophic lateral sclerosis: Moving towards a new classification system. The Lancet Neurology, 15(11), 1182-1194. https://doi.org/10.1016/S1474-4422(16)30199-5
Aldana, J. M., Álvarez, J. M., Arispón, C., Barrera, J. M., Barrot, E., & Boceta, J. (2012). Guía asistencial de esclerosis lateral amiotrófica. Sevilla: Servicio Andaluz de Salud. https://www.juntadeandalucia.es/organismos/saludyfamilias/areas/calidad-investigacion-conocimiento/calidad-sistema-sanitario/paginas/guia-ela.html
Barrera, J. M., Boceta, J., Benítez, J. M., Caballero, C., Camino, R., & Díaz, P. (2017). Documento de Consenso para la atención a los pacientes con Esclerosis Lateral Amiotrófica. Lateral Amiotrófica. Servicio Andaluz de Salud. Consejería de Salud y Bienestar Social. Junta de Andalucía. http://www.elaandalucia.es/WP/wp-con-tent/uploads/GUIA-ASISTENCIAL-ELA -revisi%C3%B3n.pdf
Barrios Osuna, I., Anido Escobar, V., & Morera Pérez, M. (2016). Declaración de Helsinki: Cambios y exégesis. Revista Cubana de Salud Pública, 42(1), 0-0. http://scielo.sld.cu/scielo.php?script=sci_abstract&pid=S0864-34662016000100014&lng=es&nrm=iso&tlng=es
Bello-Haas, V. D. (2018). Physical therapy for individuals with amyotrophic lateral sclerosis: Current insights. Degenerative Neurological and Neuromuscular Disease, 8, 45-54. https://doi.org/10.2147/DNND.S146949
Cañadilla, Y., Aguilera, M. Y., Cañete, A. C., & Aguilar, E. M. (2019). Ejercicios físico-terapéuticos, ejercicios respiratorios y apoyo nutricional en pacientes con diagnóstico de Esclerosis Lateral Amiotrófica. 609-617. La Habana, Cuba.
Desport, J. C., Preux, P. M., Truong, T. C., Vallat, J. M., Sautereau, D., & Couratier, P. (1999). Nutritional status is a prognostic factor for survival in ALS patients. Neurology, 53(5), 1059-1063. https://doi.org/10.1212/wnl.53.5.1059
Díaz-Gómez, M. F., & Ortiz-Corredor, F. (2017). Diseño y validación de un sistema de clasificación para evaluar el grado de discapacidad de los pacientes con esclerosis lateral amiotrófica. Revista de Neurología, 64(03), 112-118. https://doi.org/10.33588/rn.6403.2016315
Galán, L., López, P., & Matías-Guiu, J. (2015). Enfermedades de las motoneuronas. Medicine, 11(78), 4678-4686. https://doi.org/10.1002/mus.20415
Johnson, E. W., & Braddom, R. (1971). Over-work weakness in facioscapulohuumeral muscular dystrophy. Archives of Physical Medicine and Rehabilitation, 52(7), 333-336. https://pubmed.ncbi.nlm.nih.gov/5565885/
Jones, K. E., Berry, T. R., Merali, A. S., & Bello-Haas, V. D. (2019). Intentions of Canadian health professionals towards recommending exercise for people living with ALS. BMC Neurology, 19(1), 204. https://doi.org/10.1186/s12883-019-1426-z
Lunetta, C., Lizio, A., Sansone, V. A., Cellotto, N. M., Maestri, E., Bettinelli, M., Corbo, M. (2016). Strictly monitored exercise programs reduce motor deterioration in ALS: Preliminary results of a randomized controlled trial. Journal of Neurology, 263(1), 52-60. https://doi.org/10.1007/s00415-015-7924-z
Matos, J. A. P., Oliviero, A., & Morín Martín, M. (2019). Enfermedades de las motoneuronas. Medicine, 12(75), 4412-4422. https://doi.org/10.1016/j.med.2019.03.022
Orridge, S., & Stebbings, E. (2013). Enfermedad de la motoneurona. En E. Stokes Stack, Fisioterapia en la rehabilitación neurológica (3rd Edición). Barcelona, España: Elsevier. https://www.elsevier.com/books/fisioterapia-en-la-rehabilitacion-neurologica/stokes/978-84-9022-306-2
Paganoni, S., Chaficb, I. K., Nanettec, J., Bedlack, R., & Carter, G. T. (2015). Atención integral de rehabilitación en todo el espectro de la esclerosis lateral amiotrófica. Neuro Rehabil, 37(1), 53-68.
Plowman, E. K., Watts, S. A., & Tabor, L. (2016). Impacto del entrenamiento de fuerza espiratoria en la esclerosis lateral amiotrófica. Nervio muscular, 54(1), 48-53.
Roche, J. C., Rojas-García, R., Scott, K. M., Scotton, W., Ellis, C. E., Burman, R., Al-Chalabi, A. (2012). A proposed staging system for amyotrophic lateral sclerosis. Brain: A Journal of Neurology, 135(Pt 3), 847-852. https://doi.org/10.1093/brain/awr351
Tookman, A. J., Hopkins, K., & Scharpen, K. (2005). Rehabilitation in Palliative Medicine, Oxford Textbook of Palliative Medicine (3 ed.; D. Doyle, G. Hanks, N. Cherny, & K. Calman, Eds.). UK: Oxford UniversityPress.
Zaldivar, T., Gutierrez, J., Lara, G., Carbonara, M., Logroscino, G., & Hardiman, O. (2009). Reduced frequency of ALS in an ethnically mixed population: A population-based mortality study. Neurology, 72(19), 1640-1645. https://doi.org/10.1212/WNL.0b013e3181a55f7b
Conflict of interests:
The authors declare not to have any interest conflicts.
Authors' contribution:
Yordán Cañadilla Barrios: Conception of the idea,
literature search and review,
instrument making,
instrument application,
compilation of information resulting from the instruments applied,
Database preparation, general advice on the topic addressed, drafting of the original (first version),
review and final version of the article,
article correction,
authorship coordinator,
Review of the application of the applied bibliographic standard.
Magda Mesa Anoceto: Statistic analysis, preparation of tables, graphs and images, review and final version of the article.
Jerry Bosque Jiménez: Instrument making, translation of terms or information obtained, review of the application of the applied bibliographic standard.
Rodolfo Ruvenio Vidaurreta Bueno: Preparation of tables, graphs and images, database preparation.
Annia Caridad Cañete Rojas: Literature search and review, compilation of information resulting from the instruments applied, database preparation, general advice on the topic addressed, Review and final version of the article, article correction.
![]()
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0
International license
Copyright (c) 2020
Yordán Cañadilla Barrios, Magda Mesa Anoceto, Jerry Bosque Jiménez, Rodolfo Ruvenio Vidaurreta Bueno, Annia Caridad Cañete Rojas