
Revista PODIUM, September-December 2020; 15(3): 694-704
Translated from the original in spanish
Physical activity and heart rate variability in patients with metabolic syndrome. Narrative review
Actividad física como medida de control autonómico en pacientes con síndrome metabólico. Revisión narrativa
A atividade física como medida de controle autonômico em pacientes com síndrome metabólica. Revisão narrativa
Héctor Fuentes Barria1*![]() https://orcid.org/0000-0003-0774-0848
https://orcid.org/0000-0003-0774-0848
Catalina González Wong2 ![]() https://orcid.org/0000-0003-0360-8567
https://orcid.org/0000-0003-0360-8567
Sebastián Urbano Cerda1 ![]() https://orcid.org/0000-0003-0508-6985
https://orcid.org/0000-0003-0508-6985
Valentina Vera-Aguirre3 ![]() https://orcid.org/0000-0003-3050-5192
https://orcid.org/0000-0003-3050-5192
Raúl Aguilera Eguía4 ![]() https://orcid.org/0000-0002-4123-4255
https://orcid.org/0000-0002-4123-4255
1Universidad Santo Tomás, Facultad de Salud. Chile.
2Universidad del Desarrollo, Facultad de Ciencias de la Salud. Chile.
3Universidad San Sebastián, Escuela de Nutrición y Dietética, Facultad de Ciencias para el Cuidado de la Salud. Chile.
4Departamento de Salud Pública, Facultad de Medicina, Carrera de Kinesiología, Universidad Católica de la Santísima Concepción. Chile.
*Correspondence author: h3ct0r.fuentes.b@gmail.com
Received: December 18th, 2019.
Accepted:
September 20th, 2020.
ABSTRACT
The metabolic syndrome considers a group of disorders that increase the risk of Chronic Noncommunicable Diseases. In this sense, prevention and treatment have focused on physical activity as an effective method to restore heart rate variability and decrease health risks. The objective of this review was to describe the behavior of heart rate variability in relation to the practice of physical activity in patients with metabolic syndrome. The metabolic syndrome has been associated with sympathetic predominance and parasympathetic withdrawal that presents a risk of Chronic Noncommunicable Diseases that can be restored with regular practice of physical activity. Physical activity can restore the heart rate variability related to the metabolic syndrome, however, other studies are required to try to explain all the conditions to which the autonomic balance responds.
Keywords: exercise; autonomic nervous system; heart rate; metabolic syndrome.
RESUMEN
El síndrome metabólico considera a un grupo de trastornos que aumentan el riesgo de padecer enfermedades crónicas no transmisibles. En este sentido, la prevención y tratamiento han centrado a la actividad física como un método eficaz para restaurar la variabilidad del ritmo cardiaco y disminuir los riesgos sobre la salud. Esta revisión se planteó como objetivo describir el comportamiento de la variabilidad del ritmo cardíaco frente a la práctica de actividad física en pacientes con síndrome metabólico. El síndrome metabólico se ha relacionado con un predominio simpático y una retirada parasimpática que presenta un riesgo de enfermedades crónicas no transmisibles que puede ser restaurada con la práctica regular de actividad física. La actividad física puede restaurar la variabilidad del ritmo cardiaco relacionada al síndrome metabólico, no obstante, se requieren de otros estudios que intenten explicar todas las condiciones a las que responde el balance autonómico.
Palabras clave: Ejercicio; Sistema nervioso autónomo; Frecuencia cardiaca; Síndrome metabólico.
RESUMO
A síndrome metabólica é um grupo de perturbações que aumentam o risco de padecer Doenças Crónicas Não Transmissíveis. Neste sentido, a prevenção e o tratamento concentraram-se na atividade física como um método eficaz para restaurar a variabilidade do ritmo cardíaco e diminuir os riscos para a saúde. Esta revisão visa descrever o comportamento da variabilidade do ritmo cardíaco em relação à prática da atividade física em pacientes com síndrome metabólica. A síndrome metabólica tem sido associada com predominância simpática e retirada parassimpática que apresenta um risco de doenças crónicas não transmissíveis que podem ser restauradas com actividade física regular. A actividade física pode restaurar a variabilidade do ritmo cardíaco, relacionada com a síndrome metabólica, no entanto, são necessários mais estudos para tentar explicar todas as condições às quais o equilíbrio autonómico responde.
Palavras-chave: exercício; sistema nervoso autonómico; frequência cardíaca; síndrome metabólica.
INTRODUCTION
The metabolic syndrome (MS) is considered a major threat to health worldwide. It is not yet clearly, however, generally considers a group of disorders that occur simultaneously increasing the risk of developing Chronic Noncommunicable Diseases (CNTD) as, heart disease, obesity, and type II diabetes, among others (Robles, & Carlos., 2013; Saboya., et al., 2016). This syndrome reports a very diverse prevalence, reaching up to 27.3 % depending on the definition used in relation to the criteria and reference values in metabolic parameters as involved (Robles, & Carlos., 2013; Saboya., et al., 2016).
Currently, the literature has widely used the time variation that occurs between consecutive heartbeats (heart rate variability) as a measure that reflects the activity of the autochthonous nervous system on the cardiac function (Espinosa-Salinas, et al., 2015; Rosales-Soto, Corsini-Pino, Monsálves-Álvarez, & Yáñez-Sepúlveda, 2016; Altini, Van Hoof, & Amft, 2017; Perrotta, Jeklin, Hives, Meanwell, & Warburton, 2017; Veloza, et al., 2019). In this sense, the variability of heart rate has allowed to register and analyze the action of the autonomous nervous system and the nervous vagal system on the cardiac function in the called autonomous balance. The autonomous balance is characterized by a decrease in the heart rate marker and an increase in its variability, while a state of imbalance is characterized by increases in heart rate and decreases in its variability, as a result of the sympathetic predominance and the withdrawal of the vagal tone involved in the physiopathology of arrhythmogenesis, sudden cardiac death, arterial hypertension, obesity and insulin resistance (Espinoza-Salinas., et al., 2015; Espinoza-Salinas, Acuña-Vera, Sánchez-Aguilera, & Zafra-Santos., 2016; Yadav, Yadav, Agrawal, Sah, & Islam., 2017; Rodríguez Pena et al., 2019; Espinoza-Salinas., González-Jurado., Burdiles-Álvarez., Arenas-Sánchez, & Bobadilla-Olivares., 2020.
At present the prevention and/or treatment of the metabolic syndrome has been centered in the use of pharmacological and non-pharmacological therapies, suggesting among the latter, the practice of physical activity and/or physical exercise as an effective way to reduce body weight and restore the sympathetic-vagal balance (Miguel Soca., et al., 2012; Álvarez, et al., 2014; Yadav, et al., 2017; Kinoshita, et al., 2018). In this sense, physical activity programs have proven to be fundamental in the prevention of chronic noncommunicable diseases related to the metabolic syndrome. However, these are still being studied, due to the lack of consensus related to the interpretations of heart rate variability as a measure of autonomous control in health and disease (Billman, Huikuri, Sacha, & Trimmel., 2015; Laborde, Mosley, & Thayer., 2017; Shaffer, F., & Ginsberg., 2017).
For this reason, the objective of this review was to describe the behavior of heart rate variability in face of physical activity in patients with MS.
DEVELOPMENT
Metabolic syndrome and autonomic balance
The metabolic syndrome is considered a great threat to health worldwide, it is not yet clearly defined because of the heterogeneity between diagnostic criteria, however, in general he considers a group of disorders that occur simultaneously increasing the risk of developing CNTD, (Robles, & Carlos., 2013; Savoy et al., 2016).
This syndrome reports a very diverse prevalence, reaching up to 27.3 % depending on the definition used in relation to diagnostic criteria and reference values (Robles, & Carlos., 2013; Saboya et al., 2016), therefore, the literature has raised the linkage of diagnostic criteria related to metabolic syndrome with the variability of heart rate, (Sheema, & Malipatil., 2015; Yadal., et al., 2017; Goit, Pant, & Shrewastwa., 2018; Sessa., et al., 2018;Triggiani., 2019; Veloza., et al., 2019) (Table 1 and Table 2).
Table 1. - Diagnostic criteria for metabolic syndrome
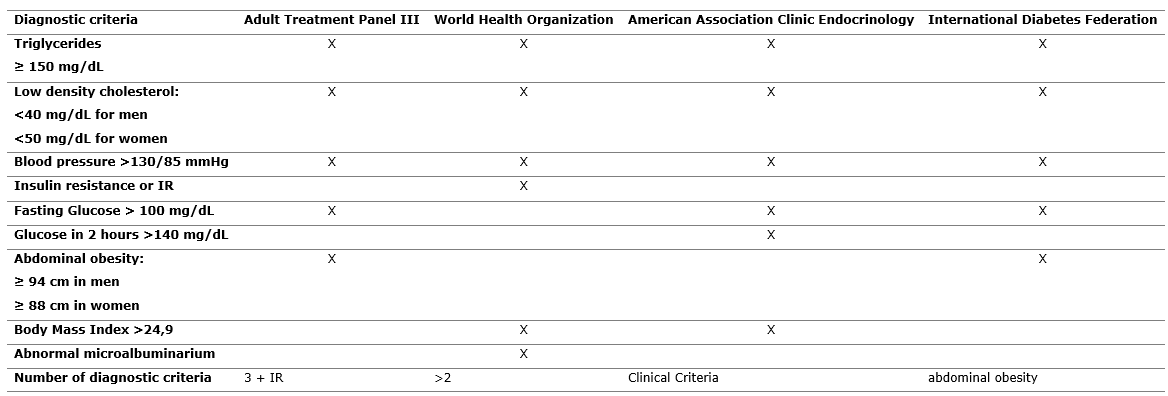
Source: Adaptation of the work of Robles & Carlos (2013)
Table 2. Main measurements of cardiac variability according to temporal, spectral and non-linear domains
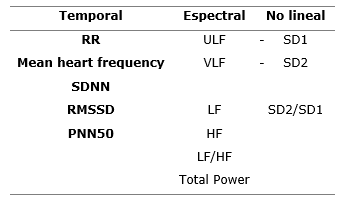
RR: Measures of the intervals R-R; SDNN: Standard deviation of all intervals RR; RMSSD: Square of the mean root of the R-R adjacent
intervals joint; PNN50: Number of the adjacent intervals that varies more than
50 ms; ULF: Ultra low frequency; VLF: Low frequency; LF: Low frequency; HF: High frequency; LF/HF: Low and high frequency relationship; SD1: Short-term variability of the heart rate; SD2: Long-term variability of the heart rate; SD2/SD1: Long-term and short term variability relationship.
Source: Adapted from the works of Tarvainen et al (2014). Triggiani et al (2016), Shaffer
& Ginsberg (2017), Rahman, Habel & Contrada (2018).
The autonomous balance is directly governed by the autonomic nervous system through its sympathetic and parasympathetic branches (Koch-Villegas., et al., 2018), so that measures of heart rate variability have allowed monitoring of the sympathetic-vagal relationship associated with the unhealthy style of life states and pathologies like, high blood pressure, insulin resistance, proliferation of adipose tissue, cardiovascular risk factors and MS (Espinoza-Salinas, et al., 2015; Sánchez, Sánchez, & Suárez, 2015; Veloza et al., 2019). In this context, a predominance in vagal activity may favor coronary irrigation, allowing a longer diastole and a shorter hypoxic period in the left ventricle, while, conversely, a sympathetic predominance is linked to increased cardiovascular morbidity and mortality regardless of the existence of other cardiovascular risk markers, such as metabolic, hemodynamic, trophic, and rheologic abnormalities (Sassi et al., 2015; León Regal et al., 2016; Wu D., et al., 2017; Rodríguez Pena, et al., 2019).
Physical activity as a measure of autonomous control
The practice of regular exercise is associated with positive adaptations in body composition, physical condition, levels of chronic inflammation and indices of heart rate variability, reflected in increases in parasympathetic tone and reductions in sympathetic activation, related to an inhibition of chronic inflammation and release of pro-inflammatory cytokines (Espinoza-Salinas., et al., 2020). In this sense, it is known that aerobic-type physical activity generates favorable changes related to autonomic restoration, mortality, inverse remodeling of the left ventricle, functional capacity and quality of life, while in physical exercise conditions around 50 % of VO2max are related to a withdrawal in the vagal activity and progressive increases of sympathetic activity. On the contrary, high intensities have been associated with an influence of the sympathetic pathway, the mechanism of synorespiratory arrhythmia and baroreflex influence in exercise conditions (García Manso., 2013; Espinoza-Salinas et al., 2016, 2020; Hernández García, et al., 2018). On the other hand, physical activity against resistance or resistance to muscle strength has been associated with a synergistic effect in terms of improvements in aerobic capacity (Hernández García., et al., 2018). Concerning physical activity against endurance or with endurance to muscular force, it has been related with a synergetic effect in order to improve the aerobic capacity and the sensitivity of baroreceptors and chemoreceptors associated to decreases in sympathetic activity directly and indirectly in resting conditions, which contributes to improve the chronotropic response to subsequent physical efforts by increasing the variability of heart rate in resting conditions. However, it is important to consider that patients diagnosed with heart failure usually present decreases in their functional capacity and tolerance to physical activity and/or exercise, so their participation in cardiac rehabilitation programs should always be considered based on the cost-benefit assessment of these programs (Segovia, Manterola, González, & Rodríguez-Núñez, 2017; Hernández García et al., 2018).
Following this line of argument, patients who performed some type of physical activity increased the magnitude of the variables of the time domain as opposed to subjects who did not receive conventional medical treatment, what suggest that the physical activity is not only limited to sympathetic-inhibitory responses, but also to parasympathetic excitatory responses in the cardiovascular control mechanisms of these patients (Segovia et al., 2017).
On the other hand, both heart rate variability and body composition have been studied separately on numerous occasions, so that there is still not an abundant literature that can explain all the modular mechanisms of autonomic balance in patients with overweight and/or obesity in conditions of rest and exercise (Sánchez, Sánchez, & Suárez, 2015). For this reason, it is important to consider the relationship between these two variables and their influence on health, since it is extremely important when making interventions both at the preventive and diagnostic levels. In this regard, the aerobic physical activity generates physiological responses modulated by sympathetic and endocrine stimuli, directly associated to the intensity of work, which also trigger other responses at the level of multiple cell lines, such as the increase in insulin sensitivity, modulation of the immune response and stimulation of endogenous antioxidant systems, modulated by the activation of AMPK and TLR-4, so that physical activity constitutes one of the main therapeutic resources used to combat obesity (Espinoza-Salinas et al., 2015; 2016; 2020).
In this context, moderate- and high-intensity physical activity is an effective way to reduce body weight and restore autonomic balance, counteracting the vagal decrease during the autonomic activation time from sensory afferences of muscle fibers type III and IV in subjects with high levels of adiposity, insulin resistance, type II diabetes and insufficiency (Miguel Soca, et al., 2012; Alvarez, et al., 2014; Yadav, et al., 2017; Kinoshita et al., 2018). As for the autonomic balance after exercise, this produces volume/pressure overload in the carotid body (main peripheral arterial chemical receptor) that stimulates the activation of baroreflex as a compensator of the blood pressure increases that induces, at first stage, of vagal decrease and a posterior decrease of the heart rate (Espinoza-Salinas., et al., 2020). This phenomenon leads to the presumption that the first phase of post-exercise recovery is modulated by the central nervous system, while the slow phase is regulated by the autonomic signals. However, some exceptions should be considered, such as subjects with high blood pressure, since they would not always achieve significant adaptations related to the restoration of the vagal autonomic balance due to the hypertensive response that makes it difficult for the heart function to adapt to minimal physical or mental stress conditions (Almeida, et al., 2017; Rodríguez Pena, et al., 2019).
On the other hand, at present, literature has postulated multiple theories that try to explain how adiposity could modify the neuronal activity involved in the autonomic nervous system and the thermogenic adaptation enhanced in conditions of weight gain both at rest and in exercise (Sheema, & Malipatil., 2015; Yadav., et al., 2017; Trigani et al., 2019). However, unfortunately all the mechanisms of sympathetic-vagal balance related to obesity, insulin resistance, and heart failure have not yet been established (Espinoza-Salinas et al., 2015; Rosales-Soto., et al., 2016; Segovia., et al., 2017; Goit, Pant, & Shrewastwa, 2018).
Autonomic balance in cardiovascular disease and obesity
Cardiovascular diseases have been related to hemodynamic changes and myocardial damage, since one of the first responses generated in these patients is the activation of afferent and efferent fibers of the autonomic nervous system, which contribute to the sympathetic-vagal imbalance, generating sympathetic activation and vagal withdrawal reflected in a decreased heart rate variability (Segovia, et al., 2017).
In this regard, a sympathetic predominance and vagal withdrawal can influence the systolic volume through variations in the contractile force and the redirection of blood flow to areas of higher vascular demand due to the stimulation of adrenergic receptors β1, β2 and β3 sensitive to adrenaline, which, in turn, trigger a series of chemical reactions on the calcium pump and the action potential of non-contractile cells in the sinus node that generate increases in heart rate and decreases in the variability of it. In contrast, a vagal predominance inhibits the sympathetic pathway resulting from activation of calcium channels and acetylcholine M1,M2,M3, and M5 receptors in the sinus node, producing decreases in heart rate and increases in heart variability of this one (Sessa et al., 2018; Veloza et al., 2019).
In this context, a predominance of sympathetic activity and vagal withdrawal could be related to a decrease in baroreflex sensitivity and metaboreceptors common to both cardiovascular disease and obesity, while the mechanisms of the autonomic balance related to the adipose tissue and the resistance to insulin have made us presume that the pro-inflammatory processes caused by the cytokines TNF- á and IL-6 and the release of hormones such as adiponectin, resistin, leptin and visfatin can cause modifications on the autonomic balance reducing the physical capacity (Espinoza-Salinas et al., 2015).
The above findings emphasize the need for future research to establish all the factors that can influence the balance of autonomy, since this knowledge is not yet clear (Rahman, Habel, & Contrada, 2018).
The excess of adiposity seems to be related to the variability of heart rate, while women seem to have a lower variability of heart rate compared to men, suggesting a protective effect against arrhythmias and against the development of coronary diseases. However, these differences are reduced throughout life due to the loss of estrogen (Sánchez, Sánchez, & Suárez., 2015). On the other hand, the most favorable cardiac variability profiles are associated with moderate and vigorous physical activity in children and adolescents with lower adiposity and better physical condition, while heart rate variability in adults and older adults is related to body composition; however, this relationship is still among said, because there is no consensus regarding the level of influence of body mass on heart rate variability, despite the fact that some research has suggested a relationship between sympathetic-vagal balance and factors such as age, sex, adiposity, sedentary lifestyle, sleep quality, and stress (Sánchez, Sánchez, & Suárez., 2015).
Most of the studies reviewed propose that sympathetic-vagal imbalances are directly related to the pathogenesis of diseases such as obesity, insulin resistance, type II diabetes, heart failure, among others related to metabolic syndrome (Espinoza-Salinas et al., 2015; Sánchez, Sánchez, & Suárez., 2015; León Regal et al., 2016; Rosales-Soto., et al., 2016; Altini, Van Hoof, & Amft., 2017; Perrotta et al., 2017; Segovia et al., 2017; Yadav et al., 2017; Wu D et al., 2017; Veloza et al., 2019; Rodríguez Pena et al., 2019; Espinoza-Salinas et al., 2020).
Finally, the findings reviewed by this review allow to better understand the behavior of the cardiac variability in the metabolic syndrome.
CONCLUSSION
Physical activity plays a fundamental role in the diagnosis, prevention and treatment of the MS, because it is capable of diminishing and even restoring the state of sympathetic-vagal imbalance. Therefore, other studies are still required to try to determine and explain all the mechanisms involved in the autonomic control in the diverse pathologies that compose the metabolic syndrome.
REFERENCES
Almeida, L. B. de, Peçanha, T., Mira, P. A. de C., Souza, L. V. de, da Silva, L. P., Martinez, D. G., et al. (2017). Cardiac Autonomic Dysfunction in Offspring of Hypertensive Parents During Exercise. International Journal of Sports Medicine, 38(14), 1105-1110. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/29050039
Altini, M., Van Hoof, C., & Amft, O. M. (2017). Relation between estimated cardiorespiratory fitness and running performance in free-living: An Analysis of HRV4Training dataIEEE International Conference on Biomedical & Health Informatics, Orlando, Florida, 249-52. Recuperado de https://ieeexplore.ieee.org/document/7897252
Álvarez, C., Ramírez Campillo, R., Henríquez Olguín, C., Castro Sepúlveda, M., Carrasco, V., & Martínez, C.(2014). ¿Pueden ocho semanas de ejercicio físico combinado normalizar marcadores metabólicos de sujetos hiperglicémicos y dislipidémicos? Revista Médica de Chile, 142(4), 458-466. Recuperado de https://scielo.conicyt.cl/scielo.php?script=sci_arttext&pid=S0034 -98872014000400007
Billman, G. E., Huikuri, H. V., Sacha, J., & Trimmel, K. (2015). An introduction to heart rate variability: Methodological considerations and clinical applications. Frontiers in Physiology, 6, 55. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/25762937
Espinoza-Salinas, A., Zafra-Santos, E., Pavez-Von Martens, G., Cofré-Bolados, C., Lemus-Zúñiga, J., & Sánchez-Aguilera, P. (2015). Análisis de variabilidad del ritmo cardiaco y su relación con la sensibilidad insulínica en pacientes obesos y con sobrepeso. Revista médica de Chile, 143(9), 1129-1135. Recuperado de https://scielo.conicyt.cl/scielo.php?script=sci_arttext&pid=S0034-98872015000900005
Espinoza-Salinas, A., Acuña-Vera, S., Sánchez-Aguilera, P., & Zafra-Santos, E. (2016). Revisión bibliográfica: efectos del entrenamiento interválico de alta intensidad en el balance autonómico y la cinética del consumo de oxígeno en sujetos obesos. Revista Horizonte Ciencias de la Actividad Física, 7(2), 30-45. Recuperado de http://revistahorizonte.ulagos.cl/index.php/horizonte/article/view/76
Espinoza-Salinas, A., González-Jurado, J., Burdiles-Álvarez, A., Arenas-Sánchez, G., Bobadilla-Olivares, M.(2020). Efectos del entrenamiento cardiovagal en la respuesta autonómica en personas con sobrepeso Effects of cardiovagal training on autonomic response in overweight people. Retos, 38, 118-122.
Goit, R. K., Pant, B. N., & Shrewastwa, M. K. (2018). Moderate intensity exercise improves heart rate variability in obese adults with type 2 diabetes. Indian Heart Journal, 70(4), 486-491. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/30170641
Hernández García S, Mustelier Oquendo J A, Larrinaga Sandrino V, Rodríguez Nande L, Sorio Valdés B, Peña Bofill V, et al.(2018). Efecto del entrenamiento físico en pacientes con insuficiencia cardiaca crónica y fracción de eyección del ventrículo izquierdo deprimida. Revista Cubana de Cardiología y Cirugía Cardiovascular, 20(3);309-328.
Kinoshita, M., Yokote, K., Arai, H., Iida, M., Ishigaki, Y., Ishibashi, S., et al. (2018). Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2017. Journal of Atherosclerosis and Thrombosis, 25(9), 846-984. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/30135334
Koch-Villegas, G., Cancino-López, J., Roco-Videla, Á., Jorquera-Aguilera, C., Aguilera-Eguía, R., & Hernández-Orellana, M.(2018). Control del ritmo cardiaco, ingesta energética y calidad del sueño en bailarines de danza clásica. Revista Finlay. 8(4), 284-290. Recuperado de http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S2221 -24342018000400006&lng=es&nrm=iso&tlng=es
Laborde, S., Mosley, E., & Thayer, J. F. (2017). Heart Rate Variability and Cardiac Vagal Tone in Psychophysiological ResearchRecommendations for Experiment Planning, Data Analysis, and Data Reporting. Frontiers in Psychology, 8, 213. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/28265249
León Regal, M., Benet Rodríguez, M., Mass Sosa, L., Willians Serrano, S., González Otero, L., & León Valdés, A. (2016). La hiperreactividad cardiovascular como factor predictivo de la hipertensión arterial en la mujer. MediSur, 14(3), 269-279. Recuperado de http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1727-897X2016000300009
Perrotta, A. S., Jeklin, A. T., Hives, B. A., Meanwell, L. E., & Warburton, D. E. R. (2017). Validity of the Elite HRV Smartphone Application for Examining Heart Rate Variability in a Field-Based Setting. Journal of Strength and Conditioning Research, 31(8), 2296-2302. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/28195974
Rahman, S., Habel, M., & Contrada, R. J. (2018). Poincaré plot indices as measures of sympathetic cardiac regulation: Responses to pychological stress and association swith pre-ejection period. International Journal of Psychophysiology: Official Journal of the International Organization of Psychophysiology, 133, 79-90. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/30107195
Robles, L., & Carlos, J. (2013). Síndrome metabólico: Concepto y aplicación práctica. Anales de la Facultad de Medicina, 74(4), 315-320. Recuperado de http://www.scielo.org.pe/scielo.php?script=sci_abstract&pid=S1025-55832013000400009&lng=es&nrm=iso
Rodríguez Pena, A., Guirado Blanco, O., González Paz, H. J., Ballesteros Hernández, M., Casas Blanco, J. C., Cárdenas Rodríguez, A. E., et al. (2019). Balance autonómico basal y durante el ejercicio isométrico en jóvenes con diferente reactividad cardiovascular. CorSalud, 11(1), 11-20. Recuperado de http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S2078 -71702019000100011&lng=es&tlng=pt.
Rosales-Soto, G., Corsini-Pino, R., Monsálves-Álvarez, M., & Yáñez-Sepúlveda, R. (2016). Respuesta del balance simpático-parasimpático de la variabilidad de la frecuencia cardíaca durante una semana de entrenamiento aeróbico en ciclistas de ruta. Revista Andaluza de Medicina del Deporte, 9(4), 143-147. Recuperado de http://scielo.isciii.es/scielo.php?script=sci_abstract&pid=S1888-75462016000400143
Saboya, P. P., Bodanese, L. C., Zimmermann, P. R., Gustavo, A. da S., Assumpção, C. M., & Londero, F. (2016). Síndrome metabólico y calidad de vida: Una revisión sistemática. Revista Latino-Americana de Enfermagem, 24. Recuperado de http://www.scielo.br/scielo.php?pid=S0104-11692016000100615&script=sci_abstract&tlng=es
Sánchez, G. F. L., Sánchez, L. L., & Suárez, A. D. (2015). Composición corporal y variabilidad de la frecuencia cardiaca: Relaciones con edad, sexo, obesidad y actividad física. SPORT TK-Revista Euro Americana de Ciencias del Deporte, 4(2), 33-40. Recuperado de https://revistas.um.es/sportk/article/view/242921
Sassi, R., Cerutti, S., Lombardi, F., Malik, M., Huikuri, H. V., Peng, C.K., et al. (2015). Advances in heart rate variability signal analysis: Joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Europace: European Pacing, Arrhythmias, and Cardiac Electrophysiology: Journal of the Working Groups on Cardiac Pacing, Arrhythmias, and Cardiac Cellular Electrophysiology of the European Society of Cardiology, 17(9), 1341-1353. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/26177817
Segovia, V., Manterola, C., González, M., & Rodríguez-Núñez, I. (2017). El entrenamiento físico restaura la variabilidad del ritmo cardiaco en la insuficiencia cardiaca. Revisión sistemática. Archivos de cardiología de México, 87(4), 326-335. Recuperado de http://www.scielo.org.mx/scielo.php?script=sci_abstract&pid=S1405-99402017000400326&lng=es&nrm=iso
Sessa, F., Anna, V., Messina, G., Cibelli, G., Monda, V., Marsala, G., et al. (2018). Heart rate variability as predictive factor for sudden cardiac death. Aging, 10(2), 166-177. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/29476045
Shaffer, F., & Ginsberg, J. P. (2017). An Overview of Heart Rate Variability Metrics and Norms. Frontiers in Public Health, 5,117. Recuperado de https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5624990/
Sheema, U. K., & Malipatil, B. S. (2015). A cross-sectional study on effect of body mass index on the spectral análisis of heart rate variability -. National Journal of Physiology, Pharmacy and Pharmacology, 5(3), 250-252. Recuperado de https://www.bibliomed.org/?mno=177891
Tarvainen, M. P., Niskanen, J.-P., Lipponen, J. A., Ranta-Aho, P. O., & Karjalainen, P. A. (2014). Kubios HRV—heart rate variability analysis software. Computer Methods and Programs in Biomedicine, 113(1), 210-220. Recuperado de https://doi.org/10.1016/j.cmpb.2013.07.024
Triggiani, A. I., Valenzano, A., Trimigno, V., Di Palma, A., Moscatelli, F., Cibelli, G., & Messina, G. (2019). Heart rate variability reduction is related to a high amount of visceral adiposity in healthy young women. PloS One, 14(9), e0223058. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/31553779
Veloza, L., Jiménez, C., Quiñones, D., Polanía, F., Pachón-Valero, L. C., & Rodríguez-Triviño, C. Y. (2019). Variabilidad de la frecuencia cardíaca como factor predictor de las enfermedades cardiovasculares. Revista Colombiana de Cardiología, 26(4), 205-210. Recuperado de https://www.elsevier.es/es-revista-revista-colombiana-cardiologia-203-articulo-variabilidad-frecuencia -cardiaca-como-factor-S0120563319300683
Wu, D., Xu, L., Abbott, D., Hau, W. K., Ren, L., Zhang, H., & Wong, K. K. L. (2017). Analysis of beat-to-beat blood pressure variability response to the cold pressor test in the offspring of hypertensive and normotensive parents. Hypertension Research: Official Journal of the Japanese Society of Hypertension, 40(6), 581-589. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/28179624
Yadav, R.L., Yadav, P.K., Yadav, L.K., Agrawal, K., Sah, SK.,& Islam, M.N. (2017). Association between obesity and heart rate variability indices: an intuition toward cardiac autonomic alteration - a risk of CVD. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy 10: 57-64. Recuperado de https://www.ncbi.nlm.nih.gov/pubmed/28255249
Conflict of interests:
The authors declare not to have any interest conflicts.
Authors' contribution:
The authors have participated in the writing of the work and analysis of the documents.
![]()
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International license.
Copyright (c) 2020
Héctor Fuentes Barria, Catalina González Wong, Sebastián Urbano Cerda, Valentina Vera-Aguirre, Raúl Aguilera Eguia