
Revista PODIUM, September-December 2020; 15(3): 494-508
Translated from the original in spanish
Therapeutic physical exercises program for amputees
Programa de ejercicios físicos terapéuticos para pacientes amputados
Programa de exercícios físicos terapêuticos para pacientes amputados
Mohamed Hosam Adeen1*![]() https://orcid.org/0000-0002-3115-696X
https://orcid.org/0000-0002-3115-696X
Jorge de Lázaro Coll Costa1![]() https://orcid.org/0000-0001-8712-2948
https://orcid.org/0000-0001-8712-2948
Ardy Rafael Rodríguez
García1![]() https://orcid.org/0000-0003-3394-5783
https://orcid.org/0000-0003-3394-5783
María Blanca García
Rubio1![]() https://orcid.org/0000-0001-7808-2913
https://orcid.org/0000-0001-7808-2913
Asunción Mayda García
Rubio1![]() https://orcid.org/0000-0002-6095-6464
https://orcid.org/0000-0002-6095-6464
1Universidad de Ciencias de la Cultura Física y el Deporte "Manuel Fajardo". La Habana, Cuba.
*Correspondence author: mohamedhosamadeen@gmail.com
Received: June 16th, 2020.
Accepted: August 12th, 2020.
ABSTRACT
The rehabilitation process for amputees lacks a methodological instrument for developing muscular strength that allows them to achieve better levels of walking and balance. For this reason, a muscle strength development program was designed to achieve better gait and balance levels for the amputee. The theoretical and methodological foundations of the rehabilitating physical treatment of the amputee patient were analyzed to establish the diagnosis of the treatment. The structure, content and methodology of the program were also determined. Which was valued by expert judgment. The study was descriptive in a holistic nature with a non-experimental design. The sample was of 19 specialists, six physiatrists with more than nine years of experience, ten rehabilitators with more than eight years of experience, an orthopedic and a Doctor of Science in Physical Culture with more than six years of experience, with an average age 45 years old, presenting a domain and level of knowledge on topic four obtained a medium and a high coefficient of 15. The applied methods were theoretical and empirical. The physical-therapeutic exercise program for amputated was structured. The experts rated the relevance and implementation of the physical-therapeutic exercise program for amputees with a strong expected effectiveness as very adequate. The preparation of the program was pertinent, since it justifies the need to guide the physical rehabilitators scientifically and methodologically. Conclusions and recommendations were reached.
Keywords: Program; Physical-therapeutic exercise; Amputee patient.
RESUMEN
El proceso de rehabilitación para los pacientes amputados carece de un instrumento metodológico para el desarrollo de la fuerza muscular que les permitan alcanzar mejores niveles de marcha y equilibrio. Por tal motivo, se elaboró un programa de desarrollo de la fuerza muscular dirigido a alcanzar mejores niveles de marcha y equilibrio del paciente amputado. Se analizaron los fundamentos teóricos y metodológicos del tratamiento físico rehabilitador del paciente amputado para establecer el diagnóstico del tratamiento. Asimismo, se determinó la estructura, contenido y metodología del programa, el cual fue valorado por criterio de expertos. El estudio fue de corte descriptivo de naturaleza holística, con un diseño no experimental. La muestra fue de 19 especialistas, seis fisiatras con más de nueve años de experiencia, diez rehabilitadores con más de ocho años de experiencia, un ortopédico y un Doctor en Ciencia de la Cultura Física con más de seis años de experiencia, con una edad promedia de 45 años, presentando un alto dominio y nivel de conocimientos sobre el tema. Los métodos aplicados fueron teóricos y empíricos. Se estructuró el programa de ejercicios físico-terapéuticos para pacientes amputados. Los expertos valoraron de muy adecuado la pertinencia e implementación del programa de ejercicios físico-terapéuticos para pacientes amputados con una efectividad esperada fuerte. Resultó pertinente la confección del programa, ya que justifica la necesidad de orientar científica y metodológicamente a los rehabilitadores físicos.
Palabras clave: Programa; Ejercicio físico-terapéutico; Paciente amputado.
RESUMO
O processo de reabilitação de pacientes amputados carece de um instrumento metodológico para o desenvolvimento da força muscular que lhes permita alcançar melhores níveis de marcha e equilíbrio. Por esta razão, foi desenvolvido um programa de desenvolvimento da força muscular para alcançar melhores níveis de marcha e equilíbrio para o paciente amputado. Os fundamentos teóricos e metodológicos do tratamento de reabilitação física do paciente amputado foram analisados para estabelecer o diagnóstico do tratamento. Do mesmo modo, a estrutura, conteúdo e metodologia do programa foram determinados e avaliados por critérios de peritos. O estudo foi descritivo e holístico por natureza, com um desenho não experimental. A amostra foi composta por 19 especialistas, 6 fisiatras com mais de 9 anos de experiência, 10 reabilitadores com mais de 8 anos de experiência, um ortopedista e um Doutor em Ciências da Cultura Física com mais de 6 anos de experiência, com uma idade média de 45 anos, apresentando um elevado nível de domínio e conhecimentos sobre o assunto. Os métodos aplicados eram teóricos e empíricos. O programa de exercícios físico-terapêuticos para pacientes amputados foi estruturado. Os peritos avaliaram a relevância e a implementação do programa de exercícios de fisioterapia para pacientes amputados com uma forte eficácia esperada. A preparação do programa foi pertinente, uma vez que justifica a necessidade de uma orientação científica e metodológica para os profissionais de reabilitação física.
Palavras-chave: Programa; Terapia de exercício físico; Paciente amputado.
INTRODUCTION
Within physical rehabilitation, as a process that is oriented towards the recovery of the patient and his or her incorporation into society in an active manner, physical exercise plays a decisive role in bringing the patient closer to the maximum limits of his or her capacity (Coll, 2012).
In Cuba, as part of the public health programs, new rooms for integral rehabilitation in primary health care have been created, which present the necessary conditions to provide a quality service to the population. In this service, specialties such as Physical Therapy and Rehabilitation, Occupational Therapy, Defectology, Speech Therapy, and Natural and Traditional Medicine are usually interrelated. Here the services of the physiotherapists graduated from Health Technology and those of the graduates of Physical Culture are interwoven, which, unlike the first ones, impregnate a pedagogical character to the process, favoring the possibilities of success in the rehabilitation of these patients.
The overall incidence of amputations is steadily rising due to higher accident rates and average life extension, which allows for the survival of elderly people with general disorders predisposing to amputation (such as peripheral ischemia). Thus, Kessler (1950) indicates that, during World War II, 18,000 American soldiers lost limbs as a result of war injuries, but in the same four-year period, 120,000 American civilians were amputated as a result of accidental injuries.
In the United States, 1 in 200 Americans has experienced a major amputation; 35,000 amputations are performed each year for congenital defects and general causes, with the most frequent location being in the lower extremities (10:3 relative to the upper extremity) (Ramos and Baryolo, 2005).
In England and Wales there are more than 80,000 people who have lost one or more members: 27,000 due to war and 60,000 due to trauma or disease. Every year about 3,500 new cases are sent to the 21 national prosthetic centers. The proportion of amputations in men is 2.5 times higher than in women, with 1 upper limb amputation for every 7 - 8 leg amputations (Ramos and Baryolo, 2005).
Of the new cases produced, 27 % are by accident, 67 % by disease and the remaining 6 % by congenital deformities. Half of the contingent of amputees registered in the current conditions are over 60 years old (Ramos and Baryolo, 2005).
In Japan, the frequency of amputations due to industrial accidents is 3.4 times higher than in the United States and the proportion of upper-extremity amputees is 14 to 10 in relation to those of lower extremities. In Spain it is estimated that the number of amputees is currently 50,000 cases (Ramos and Baryolo, 2005).
In Cuba, in the statistical report of the national institute of angiology and vascular surgery (INACV) for the year 2010, it was reported that, of the 1460 operations carried out, 320 were amputations, with more than 60 % being provided by the services of care for the diabetic (López, Triana and Pantaleón, 2013).
Of particular importance in the context of physical rehabilitation is the work to be done with amputee patients as a final alternative to a treatment process generated by the impairment of a limb. The impossibility to restore or incorporate an affected limb to a level compatible with the life of the tissues, constitutes the fundamental reason for amputations and, consequently, for the transformation of the surgeon's initial objective of saving the limb.
The rehabilitation of the amputee can be analyzed from two points of view. On the one hand, it constitutes the use of all the medical tools that can favor recovery, where the medical means belong, above all, to the field of physical medicine and are used as a supplement to the medical and surgical treatments used. On the other hand, it is conceived as the restoration of the invalid to its maximum limits in the physical, mental, social, vocational and economic order possible (Ramos and Baryolo, 2005).
Amputee patients come to receive specialized care from general primary health care services where specialized personnel are available to provide effective rehabilitation. Although the rehabilitation process of amputee patients is based on a comprehensive concept that includes physical aspects, there is a lack of an instrument specifically designed for the development of muscle strength to achieve better levels of walking and balance.
In this sense, a program for the development of muscular strength was elaborated, aimed at reaching better levels of walking and balance of the amputee patient.
MATERIAL AND METHODS
The study was of a descriptive nature of a holistic nature with a non-experimental design. By means of the intentional selection criterion, which in turn is part of the inclusion criterion, the amputees with unilateral lower limb infracondylea and supracondylea with associated diseases, with an average age of 55 to 83 years, were chosen. The sample consisted of 30 patients.
Besides, it was selected a sample of 19 specialists, six physiatrists with more than nine years of experience, ten rehabilitators (six Graduates in Physical Culture and four Health Technologists) with more than eight years of experience, an orthopedic doctor and a Doctor in Science of Physical Culture with more than six years of experience, with an average age of 45 years, presenting a good domain and level of knowledge on the subject (four obtain medium coefficient and 15 high).
The theoretical method analytical-synthetic was applied: it allowed the decomposition of the rehabilitation process of the amputated patient in the primary health care, to conceive the main elements that conform it in order to determine its particularities and to integrate it, and it allowed discovering relations and arriving at the general characteristics.
Among the empirical methods carried out are:
Consultation of official documents: this method made it possible to carry out a synthesis of existing programs, clinical histories and medical indications made by specialists, to characterize them and to arrive at establishing the methodological indications for the preparation of a rehabilitation treatment program for amputee patients.
Structural-functional systemic: it was applied to the object of study and the field of action to establish the components, structure and methodology of the program.
Expert criteria: it allowed experts to evaluate the program through their knowledge and make their judgment based on categories.
Chanlat matrix: was used from the assessment of the 19 experts to evaluate the expected effectiveness of the program (EEP) and allowed to assess the impact, functionality and opportunities provided by the program, which is expressed in the degree it has for its application and generalization.
To elaborate the physical-therapeutic exercise program, the structure applied by Fernández (2011) was assumed and it was conceived in a period of two years. The distribution of the contents is carried out according to the different stages through which the program passes, being modified in the following way: foundation, general objective, diagnosis, stages, contents organized by stages, control and evaluation and methodological indications.
Procedure
The research was carried out in the four polyclinics of integral rehabilitation in the primary health care of the Cerro municipality. The contents of the official documents, the patients' clinical records and the most recent research were systematized. There were analyzed eight theses distributed in: two diploma works, two theses in option to the scientific title of master and four doctoral theses, which provided necessary elements for the elaboration of the program.
The program was subjected to an evaluation by the experts, where each one of them issued their judgment according to the sources of argument: theoretical analyses carried out by you, experience obtained, works of national and foreign authors, knowledge of the current state of the problem abroad and the institution, with attention to the degree of influence of each one of the sources on its criteria HIGH (A), MEDIUM (M) and LOW (B) which are related to the value of the coefficient of competence K which is in the range 0. 25 ≤ K ≤ 1 and is evaluated as follows (Crespo, 2007):
Kc coefficient is calculated according to the opinion of the possible expert about his level of knowledge about the problem being solved and with the sources that allow him to argue his criteria, through the mathematical equation K = 1/2 (Kc + Ka), where Kc is the coefficient of knowledge or information that the expert has about the problem, calculated on the basis of the self-evaluation he makes on a scale from 0 to 10 and multiplied by 0. 1 (divided by ten) so that the evaluation 0 indicates absolute ignorance of the problem being evaluated and the evaluation ten indicates full knowledge of the referred problem Crespo (2007).
RESULTS AND DISCUSSION
Physical therapeutic exercise program for amputee patients
Amputation is a medical entity of a special nature because the disability is a result; not of a form of pathology; but of a form of treatment that has eliminated the pathology. The inability to restore or incorporate an affected limb to a level compatible with tissue life is the fundamental reason for amputations and, consequently, for the transformation of the surgeon's initial objective of saving the limb. The program is aimed at 30 amputee patients, who perform physical activity in primary health care centers, in order to develop muscle strength capacity.
Program foundation
The essential theoretical sources on which the program is based are the criteria provided by (Verjoshansky, 1990; Hartmann and Tunnemann, 1993 and Bompa, 2005) supported by the knowledge of Moore (1980) and the theory of sports training of Matveev (1995) where the system of principles that support the development and application of the program is derived. In which, the process of the physical rehabilitation of the amputee patient is supported on the physical exercises and on the theoretical foundations of the therapeutic physical culture and of the integral rehabilitation (WHO, 1969) quoted by (Rodríguez, 2017).
General objective
Developing muscle strength capacity in amputees to facilitate the restoration of their motor and functional condition.
Diagnosis
Objective: establish the characteristics of amputee patients who are incorporated into the strength program.
Action I: Interview
Operations:
Action II: physical examination
Operations:
Program stages:
Content of the program organized by stages: the content of the program is focused on three stages: Basic physical preparation, Pre-prosthetic strengthening, Stabilization or Prosthetic, which are closely related and characterized by the fulfillment of the principles mentioned in the foundation and by the systemic character of the same.
The described monthly measurements are made with the objective of adjusting the loads by levels and objectives identified for each patient.
In addition, it is necessary to take into account the levels of assimilation determined through the anamnesis given by the categories of beginner, intermediate and advanced, which will be differentiated between them by the duration of each session, the number of weekly sessions and the development of motor skills presented by each patient. All this is closely related to the content of each stage, that is, in each one of them each level of assimilation will be characterized (beginner, intermediate and advanced), in such a way that the teacher can perfectly individualize the loads and work according to the principles assumed to base the existence of this program.
First stage: basic physical preparation
Objective: achieve overall physical development of the muscle strength and endurance capacity of the amputated limb and healthy limbs of amputees.
Operations:
Exercises performed at this stage: passive mobilizations (relaxed and forced), active mobilizations (free, resisted and assisted), exercises for general physical development.
Second stage: pre-prosthetic strengthening
Objective: increase overall physical development of muscle strength and endurance of the amputated limb and healthy limbs of amputees and prepare them for fitting the prosthesis.
Operations:
Recovery of strength will be essential to prepare the amputated limb for the prosthesis and to perform transfers when the patient is not wearing the prosthesis.
Exercises performed at this stage: strengthening exercises for all muscle levels. Coordination exercises. Standing up and sitting down. Standing and transferring body weight to the prosthesis and maintaining balance. Exercises to improve functionality.
Third stage: stabilization or prosthetics.
Objective:
Operations:
Exercises performed at this stage: exercises in the parallel lines (balance, strength, coordination and walking. Static and dynamic patterns of walking). Walking outside the parallel bars (first with several supports and then with as little support as possible) (balance, strength, coordination and walking. Static and dynamic patterns of the march). Exercises in free areas (grass, sand, ascents, descents and stairs) Strength exercises for the stump.
Evaluation and control system
Control:
Evaluation
Initial examination of the patient: through this exploration, the rehabilitator will carry out an examination of the patient's physical condition in terms of joint mobility and amplitude, strength in both the healthy members and the amputated member, the activities that the patient is able to perform, either with assistance or alone. Patients are evaluated at the beginning of their rehabilitation.
The following tests can be performed:
Methodological indications to be taken into account
For the above mentioned, some considerations are suggested for the application and dosage of the exercises, where the rehabilitator must take into account:
The treatment session lasts approximately 60 to 90 minutes, divided into three parts: the initial part which constitutes a moment for the preparation of the patient, this initial part lasts 10 to 15 min where the blood pressure and pulse are controlled. Then follows the main part, which is where the objectives of the session are met. It lasts between 45 and 65 minutes and ends with the final part of the session, which is a moment when the patient recovers from the main part. In this third part the pulse and blood pressure are also controlled, lasting between five and ten minutes.
Number of repetitions to be used in total: it must be taken into consideration that only one weight will be used in each exercise, since it is very difficult at the beginning to change the constant weight, the following number of repetitions can be done:
The dosage of the load would be as follows:
The batches to be used would be as follows:
Gradual increase in the complexity of the exercises: the exercises described and illustrated in the program were selected and placed in the respective stages of the program in such a way that they increased in complexity and integration of the motor responses, without losing sight of the physical conditions that represent the passage of the fundamental positions.
All the experts think that the proposed program has a lot of relevance given its importance and social usefulness, seven of them express their answers to give relevance to the need for it in primary health care. The exercises were considered very adequately described and illustrated by 73.68 % of the experts, quite adequately by 21.05 % and adequately by only one expert (5.26 %). With regard to muscular strength exercises, they were considered very appropriate by 89.47 % and quite appropriate by 10.52 % of the experts.
There was consensus in considering the program's evaluation and control system to be very adequate and quite adequate. Criteria were used to refine the methodological indications, and above all it was necessary to expand them and write them down with greater precision.
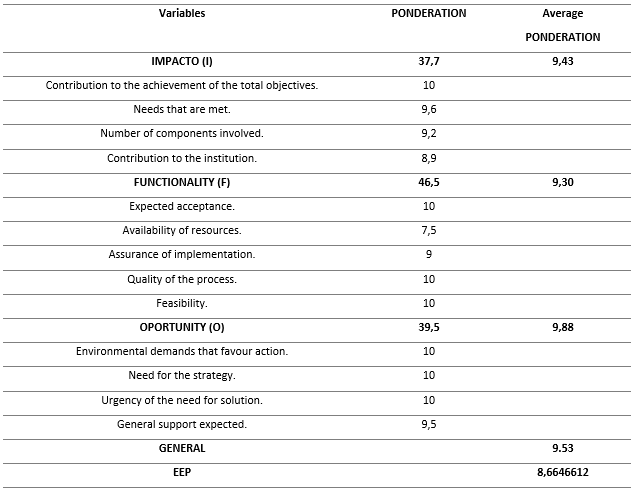
The Chanlat matrix was used based on the experts' assessment, which makes it possible to identify the strengths and weaknesses of the proposal; as for the variables (Impact, Functionality and Opportunity) they expressed their judgment to evaluate the expected effectiveness of the program (EEP).
According to Bringas and Paulas, cited by (González, 2014 and Rodríguez, 2017), this technique makes it possible to identify the potentialities and insufficiencies of any proposal that is built from a referential theoretical framework, where the sciences and the theoretical referents expose the constancies and evidences in the theoretical and practical contributions (Rodríguez, 2017).
The analysis of the results of the EEP, as shown in Figure 1, yielded about 8.66 points out of a maximum of 10, which means that the program for application in amputee patients is considered strong, being relevant if applicable in social practice, which favors and enriches the comprehensive physical rehabilitation in this type of population. This result coincides with those found by Bringas and Paulas, cited by (González, 2014 and Rodríguez, 2017) (Table 1).
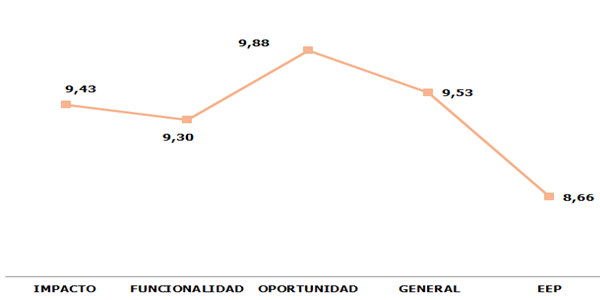
Fig.1 - Expected program effectiveness
Table 1. - Chanlat Matrix results
In conclusion, the process of physical rehabilitation of the amputee patient was based on physical exercises and the theoretical foundations of therapeutic physical culture and comprehensive rehabilitation (WHO, 1969) cited by (Rodriguez, 2017). It was diagnosed the current state of the physical rehabilitation process of the amputee patient, lacking a program to develop muscle strength to achieve better levels of walking and balance. The physical-therapeutic exercise program for amputee patients was structured in accordance with Fernandez's (2011) criteria for adjusting its methodology. The experts assessed the relevance and implementation of the physical therapy exercise program for amputee patients with a strong expected effectiveness as very appropriate.
REFERENCES
Bompa, T. (2005). Periodización del entrenamiento deportivo (La nueva onda en el entrenamiento de fuerza). Recuperado de: http://www.sobreentrenamiento.com/publice/articulo.asp?ida=188.
Crespo, B.T. (2007) Respuesta a 16 Preguntas sobre el empleo de expertos en la investigación pedagógica. Editorial San Marcos, Lima. Perú. Primera Edición. Disponible en: https://www.researchgate.net/publication/324823013_RESPUESTAS_A_16_PREGUNTAS_SOBRE_EL_EMPLEO_DE_EXPERTOS_EN_LA_INVETIGACION_PEDAGOGICA
Coll, J.L. (2012). Programa de ejercicios físicos terapéuticos para la rehabilitación de pacientes hemipléjicos en la atención primaria de salud. [Tesis doctoral]. La Habana: Universidad de Ciencias de la Cultura Física y el Deporte Manuel Fajardo. Disponible en: https://www.semanticscholar.org/paper/Programa-de-ejercicios-f%C3%ADsicos-terap%C3%A9uticos-para-la-Costa-L%C3%A1zaro /58c21e803c43e82bfcf43514432508498be88c7f
Hislop, H.J. y Montgomery, J. (2003) Daniels & Worthingham. Técnicas de Balance Muscular. Editorial Elsevier, Madrid España. Séptima Edición. Disponible en: https://www.sciencedirect.com/book/9788490225059/daniels-y-worthingham-tecnicas-de-balance-muscular
Fernández, A.L. (2011). Propuesta de un programa de ejercicios físicos para la rehabilitación de pacientes con afecciones motrices por accidentes cerebrovasculares. EFDeportes.com, Revista Digital. Buenos Aires Año 16 - Nº 157. Disponible en: https://www.efdeportes.com/efd157/rehabilitacion-de-accidente-cerebrovascular.htm
González, K. (2014) Programa de acondicionamiento físico dirigido a la población adulta joven que asiste a los gimnasios de cultura física. Articular [Tesis doctoral]. La Habana: Universidad de Ciencias de la Cultura Física y el Deporte Manuel Fajardo. Disponible en: http://eduniv.mes.edu.cu/bd/td/Gonzalez%20Acosta%2C%20Kenia /Programa%20de%20acondicionamiento%20fisic%20%28653%29/Programa%20de%20acondicionamiento%20f%20-%20Gonzalez%20Acosta%2C%20Kenia.pdf
Hartmann, V. y Tunnemann, H. (1993). Entrenamiento moderno de la fuerza. Editorial Paidotribo. Disponible en: https://dialnet.unirioja.es/servlet/libro?codigo=170238
Kessler, H. (1950). Handbook of physical medicine and rehabilitation. American Medical Association. Disponible en: https://books.google.com.cu/books/about/Handbook_of_Physical_Medicine_and_Rehabi.html?id=2sLvNV58V8oC&redir_esc=y
López, S., Triana, M, E. y Pantaleón, O, S. (2013). Comportamiento de las amputaciones mayores causadas por enfermedad vascular periférica durante un semestre. Revista Cubana de Angiología y Cirugía Vascular 2013; 14 (2). Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=44896
Matveev, L.P. (1995). Teoría del deporte. Editorial Digeder. Moscú. Disponible en: https://www.libreriadeportiva.com/libro/teoria-del-deporte_20772
Moore, J. (1980). Neuroanatomical considerations relating to recovery of function: Theoretical consideration for brain injury rehabilitation. Verlag: Ed. Bach-y-Rita. Hans Huber Publis-hers; p.9-90.
Ramos, R. y Baryolo, A. (2005). Rehabilitación del Amputado de Miembro Inferior. Recuperado de: Medicina de Rehabilitación Cubana. Camagüey, Cuba. Recuperado de: http://www.sld.cu/galerias/pdf/sitios/rehabilitacion-bio/manual_de_amputados.pdf
Rodríguez, G.A. (2017). El ejercicio físico-terapéutico en pacientes adolescentes con Síndrome de Hipermovilidad Articular [Tesis doctoral]. La Habana: Universidad de Ciencias de la Cultura Física y el Deporte Manuel Fajardo.
Verjoshansky, Y. (1990). El entrenamiento deportivo. Planificación y programación. Barcelona, Editorial Martínez Roca. Disponible en: https://books.google.com.cu/books/about/Entrenamiento_deportivo_planificacion_y.html?id=EWqwAAAACAAJ&redir_esc=y
Conflict of interests:
The authors declare not to have any interest conflicts.
Authors' contribution:
The authors have participated in the writing of the work and analysis of the documents.
![]()
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International license.
Copyright (c) 2020
Mohamed Hosam Adeen, Jorge de Lázaro Coll Costa,
Ardy Rafael Rodríguez García, María Blanca García Rubio, Asunción Mayda García Rubio