
PODIUM. Journal of Science and Technology in Physical Culture, September-December; 16(3): 757-771
Translated from the original in spanish
Methodology for conventional gait training in patients with spinal injuries. Preliminary study
Metodología para el entrenamiento de la marcha convencional en pacientes con lesiones medulares. Estudio preliminar
Metodologia para o treinamento de marcha convencional em pacientes com lesões medulares. Estudo preliminar
Alexander Echemendia del Valle1*![]() https://orcid.org/0000-0001-8737-2269
https://orcid.org/0000-0001-8737-2269
1International Center for Neurological Restoration (CIREN). Cuba.
*Corresponding author: alex@neuro.ciren.cu
Received: 07/09/2020.
Approved: 19/07/2021.
ABSTRACT
Spinal cord injury is a complex medical condition that disrupts the lives of people who suffer from it, those affected become dependent due to the multiple sequelae that accompany it, among which the loss of gait stands out, standing as one of priorities in neurorehabilitation. Most international neurorehabilitation programs do not include a defined methodology for gait recovery in spinal cord injured patients. Specialists from the International Center for Neurological Restoration created a methodology for this purpose. The objective of the study was to verify the behavior of the application of the methodology with a sample of 5 patients treated at the institution using content analysis, observation and measurement methods. The patients in the sample were evaluated before and after applying the methodology with the SCIM III, WISCI II scales. Treatment lasted 8 weeks for each patient. The results showed an increase in the functional capacity of walking in the patients, without the presence of complications. It is assumed that the use of the methodology can guarantee a functional process for gait training, in an organized manner in patients with spinal cord injuries.
Keywords: Neurology; Spinal cord injury; Neurorehabilitation; Gait.
RESUMEN
La lesión de la médula espinal es un estado médico complejo que trastorna la vida de las personas que la padecen, los afectados pasan a ser dependientes por las múltiples secuelas que le acompañan entre las que se destaca la pérdida de la marcha, erigiéndose como una de las prioridades en la neurorrehabilitación. La mayoría de los programas internacionales de neurorrehabilitación no incluyen una metodología definida para la recuperación de la marcha de los pacientes lesionados medulares. Los especialistas del Centro Internacional de Restauración Neurológica crearon una metodología con este fin. El objetivo del estudio fue comprobar el comportamiento de la aplicación de la metodología, con una muestra de cinco pacientes atendidos en la institución y se utilizaron métodos de análisis de contenido, observación y medición. Los pacientes de la muestra se evaluaron antes y después de aplicada la metodología con las escalas SCIM III, WISCI II. El tratamiento duró ocho semanas para cada paciente. Los resultados mostraron un incremento de la capacidad funcional de la marcha en los pacientes, sin la presencia de complicaciones. Se presupone que el empleo de la metodología puede garantizar un proceso funcional para el entrenamiento de la marcha, de forma organizada en pacientes lesionados medulares.
Palabras clave: Neurología; Lesión medular; Neurorrehabilitación; Marcha.
RESUMO
A lesão medular é uma condição médica complexa que perturba a vida das pessoas que sofrem com ela, e os afetados se tornam dependentes devido às múltiplas seqüelas que a acompanham, entre as quais se destaca a perda da caminhada, tornando-a uma das prioridades na neuroreabilitação. A maioria dos programas internacionais de neuroreabilitação não inclui uma metodologia definida para a recuperação de pacientes com lesões da medula espinhal. Os especialistas do Centro Internacional de Restauração Neurológica desenvolveram uma metodologia para este fim. O objetivo do estudo foi testar o comportamento da aplicação da metodologia, com uma amostra de cinco pacientes tratados na instituição, utilizando métodos de análise de conteúdo, observação e medição. Os pacientes da amostra foram avaliados antes e depois da aplicação da metodologia com as escalas SCIM III e WISCI II. O tratamento durou oito semanas para cada paciente. Os resultados mostraram um aumento na capacidade de marcha funcional dos pacientes, sem a presença de complicações. Assume-se que o uso da metodologia pode garantir um processo funcional para o treinamento da marcha de forma organizada em pacientes lesionados pela medula espinhal.
Palavras-chave: Neurologia; lesão medular; Neuroreabilitação; Andamento.
INTRODUCTION
Despite advances in medical science, spinal cord injury continues to be one of the most devastating clinical situations, both because of the functional loss it entails and, consequently, the loss of independence of the individual, and because of the limited possibilities of spontaneous recovery coupled with the lack of curative treatment. Although in recent decades, knowledge in the care of spinal cord injury has evolved significantly, spinal cord injury continues to pose a serious problem from social, economic and physical points of view (Andrade et al., 2019; Barclay et al., 2019; McDaid et al., 2019; Miller et al., 2016; Sutton et al., 2020).
Currently, research is directed towards regeneration (Babaloo et al., 2019), neuroprotection (Sandrow-Feinberg & Houlé, 2015) and medullary plasticity (Hutson & Di Giovanni, 2019), it is sought, above all, to diminish the neurological sequelae left by the disease.
Spinal cord injury affects a small but significant portion of the population. In reviewing all causes of disability in the U.S. from 1976-1980, the rate of spinal cord injury was found to be 17 per 100,000 populations with an average age of 12-42 years and approximately 10,000 new spinal cord injuries typically occur each year (Hidalgo Martinez, 2017).
Treatment is based on the coordination of a group of specialized professionals: doctors, nurses and health professionals among which physical rehabilitation specialists stand out, headed by Physical Culture Graduates and Rehabilitation Technicians who provide optimal care, thanks to the experience of specialized centers and groups committed and trained to provide continuity of care from the place of the accident and throughout the life of the spinal cord injured person. The elements of this therapeutic approach are based on prevention, pre-hospital care, acute care, rehabilitation and lifelong medical follow-up (Miller et al., 2016). Although in recent years it has been the focus of study with technological advances such as nanotechnology or robotics (Holland et al., 2017; Mekki et al., 2018) and scientific advances, such as the application of stem cells with great results in the reconstruction of nerve tissue (Chasman et al., 2019).
In neurorehabilitation, gait training in spinal cord injuries is adapted to the existing residual musculature, so that the type of gait to be achieved, the orthosis and the technical aids for walking (walker or Canadian canes) depend on the strength present in the different muscle groups. The physical work is aimed at working on or re-educating the most important determinants of walking, i.e. maintaining or releasing joint arches, strengthening the musculature, controlling high tone and re-educating coordination and balance. While specifically working on the gait determinants, compensatory strategies are developed that facilitate movement according to the limitations (Holanda et al., 2017; Mazzoleni et al., 2017).
Depending on the level of injury and the functioning muscle groups, the following phases can be progressed through: passive standing, parallel balancing, parallel walking, walking with a walker, walking with a cane in parallel, off-parallel cane balancing, off-parallel cane walking, stairs, and outdoor walking (Chisholm et al., 2019; Midik et al., 2020; Okawara et al., 2020).
In the world, there are many centers dedicated to the rehabilitation of spinal cord injured patients, some with vast experience in this specialty and with established programs, examples of them are the works of Hidalgo Martínez in which the impact of technologies in spinal cord injury is addressed (Hidalgo Martínez, 2017), the methodological conception for hydrokinesitherapy raised by Dra. Lesbia (Jiménez-Pascual, 2013), or the Exercises and methodology for teaching walking by Silverio and Lidia for paraplegics (Silva & Rodríguez, 2004).
All of them have in common that their approach is carried out from the field of Physical Culture and are based on pedagogical conceptions that enrich the rehabilitation process, although in no case is a uniform methodology shown for the functional recovery of walking in these patients. The International Center for Neurological Restoration of Cuba (Ciren in Spanish) recently created a methodology for this purpose to be added to its Physical Rehabilitation Program for spinal cord injured patients. The objective is to evaluate in a preliminary way the behavior in the functional capacity of walking of spinal cord injured patients, when applying the methodology for the training of conventional walking elaborated in Ciren.
MATERIALS AND METHODS
Type of study: longitudinal, prospective, quasi-experimental study. In the present study, a single group was followed.
Population: patients admitted to the Clinic of rachimedullary affections, neuromuscular diseases and multiple sclerosis of the International Center of Neurological Restoration, Havana, Cuba, carriers of spinal cord injuries.
Sample: five patients, three women and two men, with spinal cord injuries at the thoracic level, TS:1; T8:1; T10:2; T12:1. The mean age was 26.6 years, with the youngest age being 18 and the oldest 34 years, with a range of 16 years, and a standard deviation of 6.804.
Methodology
The methods used were:
Qualitative order
Quantitative
The experiment was organized with the following steps.
a) The sample was randomly selected and met the following inclusion criteria:
Edinburgh, Scotland: 52nd General Assembly 2000").
Output criteria:
b) Application of the initial evaluation of the selected patients using the instruments:
From the SCIM III scale, some items related to other activities were excluded and only the analyzed mobility items were analyzed (indoor and outdoor, on any surface), which evaluate the patient's gait in certain environments with levels of complexity that allow the Physical Culture specialist to foresee the displacement capacity that a patient can achieve, as well as the reduction of barriers that allow his or her social integration.
The WISCI II scale was used in its entirety since it is a scale created to evaluate the gait of the spinal cord injured patient and its score ranges from 0 to 20.
c) Application of the methodology for gait training: which consisted of the application of the methodology by 2 neurorehabilitation specialists, selected for 8 weeks for each patient, with the following organization by stages:
Stage 1. Stratification
Objective. To determine the functional status of the patient who begins the rehabilitation process.
Procedures
Table 1. - Functional group based on gait

RESULTS AND DISCUSSION
Methodological guidelines according to the procedure
To perform this evaluation, the indications and contraindications described for these tests in general (Ditunno et al., 2013) were taken into account. Some of these indications and contraindications are outlined below.
Stage 2. Intervention
Objective. To implement the contents to be developed in the training session.
Procedures
Methodological indications according to the procedure
Contents and methodological recommendations for the training session
It begins with stretching and joint mobility exercises, which should take approximately five to ten minutes. Before starting the warm-up, the training pulse and respiratory rate should be checked. To start the training session:
There must be a correspondence between the necessary increases in the stimulus of the workload, with the physiological and clinical responses of the patient in order to progressively achieve the improvement of muscular strength and endurance, as well as functional capacity without risks or complications that could lead to interrupting or terminating it.
General indications for walking activities
General data of the activity
Stage 3. Functional assessment
Procedures
Methodological indications according to the procedure
1. Check the rehabilitation file for attendance at physical rehabilitation sessions. In case of interruptions, to mention the reasons.
2. Verify that the indications in terms of intensity and dosage for each functional group have been complied with and that there was tolerance and adaptation to the loads.
3. Carry out the corresponding functional evaluation to assess the results of the stage worked on and decide on the strategy and/or readjustment in order to continue improving the functional walking capacity achieved by the patient.
Indicators for moving between stages
Indicators that allow the transition from the second to the third stage
d) Final evaluation of the patients, which was carried out under the same conditions as the initial evaluation and by the same evaluators.
e) Collection, processing and analysis of the results. Descriptive statistics was applied, using the median as a measure of central tendency and the standard deviation as a measure of dispersion for each parameter. In addition, for the analysis of qualitative variables, the Wilconxon test for related samples was used. The significance level used was p<0.05.
All the procedures used in the research were approved by the scientific committee of the Rehabilitation Center and Ciren.
The results obtained by patients in the different tests are shown below (Figure 1), the descriptive statistics of the gait and mobility scales at the beginning and end of the experiment (Table 2), the comparison of the initial values with the final values in gait and mobility (Table 3) and the Functional Assessment (Table 4) in which the functional evolution of each patient is observed.
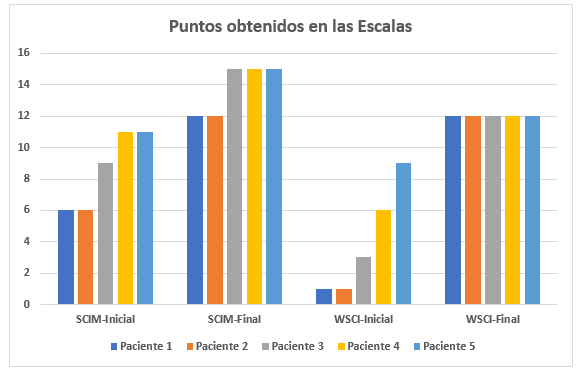
Fig. 1. - Comparison of applied scales
Figure 1 shows the results obtained by the patients in the mobility and gait tests individually.
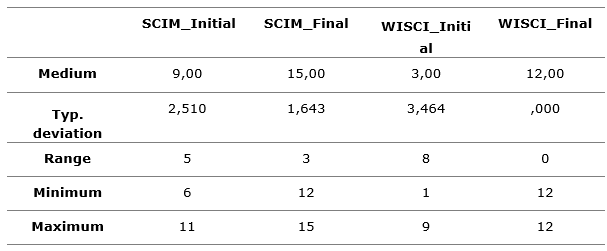
Table 2 shows the descriptive statistical data of the mobility and gait tests, analyzed as a group, carried out at the beginning and end of the patients' treatment period. The most relevant thing that is observed in both tests is an improvement in the gait parameters of the final values in terms of the median, it is also observed that the dispersion of the data decreases in both tests, also decreasing the range between the maximum and minimum values of the sample (Table 2).
Table 2. - Descriptive statistics
To verify the hypothesis of the research, the Wilconxon non-parametric test was performed with a significance level of p< 0.5 (Table 3), where it is clearly observed that, in both tests, statistically significant changes are obtained, from which it can be inferred that the improvement obtained by the patients in walking is due to the introduction of the methodology and not to chance.
Table 3. - Contrast statisticsa
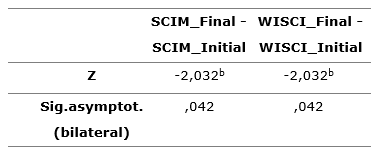
a. Wilcoxon signed-rank test
b. Based on negative ranges.
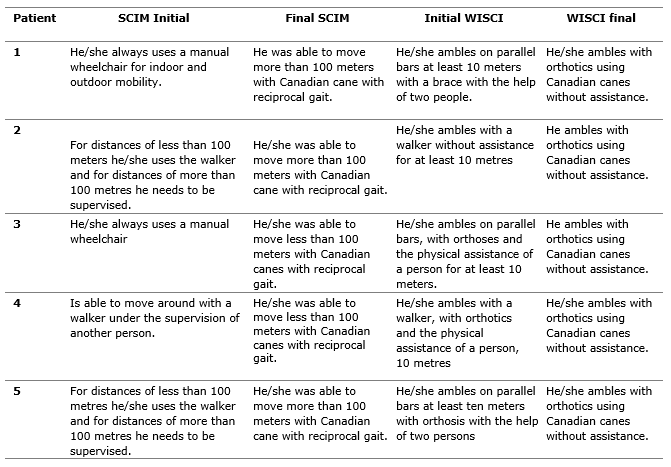
Table 4 shows in a functional way how each patient evolved in walking, when applying the instruments, highlighting that all patients, in the scale that evaluates mobility, were able to move with Canadian canes, at least for moderate distances between 10 and 100 meters and in the walking scale itself (WISCI III), all patients were able to move with Canadian canes and orthosis without the help of any person.
Table 4. - Functional assessment of the patients
The applied methodology guaranteed a logical functional process for gait training, in an organized and structured way, which allowed establishing a common work guide for all the rehabilitators of the International Center of Neurological Restoration that attends spinal cord injured patients. The results of the preliminary study showed an increase in the functional capacity of gait in patients, without the presence of complications.
All patients met the target within 8 weeks. Of the five patients studied, 3 (60 %) were able to walk more than 100 meters using the Canadian canes, according to the final SCIM scale. All five patients, 100 %, were able to amble the distance covered with the Canadian canes and with orthoses, without the assistance of another person, as shown by the final WISCI scale.
With this study, it was possible to prove that when it is had the selected instruments for gait assessment (SCIM III and WISCI II) and it is had an adequate training program, satisfactory results can be obtained as shown by different studies (Calhoun Thielen et al., 2017; Mulcahey et al., 2016). Another achievement of the study is to highlight the positive changes that can be obtained in patients through intensive physical exercise, in patients with spinal cord injury, supported by different studies (Gaspar et al., 2019; Hicks, 2020) and what may represent the achievement of greater independence for the quality of life of patients, obtained by other researchers (Amtmann et al., 2019; Ribeiro Neto et al., 2020). The application of this methodology, with a greater number of patients in different neurorehabilitation contexts and by other specialists in physical neurorehabilitation, presupposes that similar results can be obtained that benefit more patients in less rehabilitation time and facilitate a guide for the work of physical therapists.
The results obtained in the research process showed the importance of the creation and application of the methodology for uniform gait training by specialists, which represents an indispensable methodological contribution in the physical rehabilitation of patients with spinal cord injuries.
REFERENCES
Amtmann, D., Bocell, F. D., Bamer, A., Heinemann, A. W., Hoffman, J. M., Juengst, S. B., Rosenberg, M., Schneider, J. C., Wiechman, S., & McMullen, K. (2019). Psychometric Properties of the Satisfaction With Life Scale in People With Traumatic Brain, Spinal Cord, or Burn Injury: A National Institute on Disability, Independent Living, and Rehabilitation Research Model System Study. Assessment, 26(4), 695-705. https://doi.org/10.1177/1073191117693921
Andrade, V. S., Faleiros, F., Balestrero, L. M., Romeiro, V., & Santos, C. B. D. (2019). Social participation and personal autonomy of individuals with spinal cord injury. Rev Bras Enferm, 72(1), 241-247. https://doi.org/10.1590/0034-7167-2018-0020
Babaloo, H., Ebrahimi-Barough, S., Derakhshan, M. A., Yazdankhah, M., Lotfibakhshaiesh, N., Soleimani, M., Joghataei, M. T., & Ai, J. (2019). PCL/gelatin nanofibrous scaffolds with human endometrial stem cells/Schwann cells facilitate axon regeneration in spinal cord injury. J Cell Physiol, 234(7), 11060-11069. https://doi.org/10.1002/jcp.27936
Barclay, L., Lentin, P., Bourke-Taylor, H., & McDonald, R. (2019). The experiences of social and community participation of people with non-traumatic spinal cord injury. Aust Occup Ther J, 66(1), 61-67. https://doi.org/10.1111/1440-1630.12522
Calhoun Thielen, C., Sadowsky, C., Vogel, L. C., Taylor, H., Davidson, L., Bultman, J., Gaughan, J., & Mulcahey, M. J. (2017). Evaluation of the Walking Index for Spinal Cord Injury II (WISCI-II) in children with Spinal Cord Injury (SCI). Spinal Cord, 55(5), 478-482. https://doi.org/10.1038/sc.2016.142
Chasman, D., Iyer, N., Fotuhi Siahpirani, A., Estevez Silva, M., Lippmann, E., McIntosh, B., Probasco, M. D., Jiang, P., Stewart, R., Thomson, J. A., Ashton, R. S., & Roy, S. (2019). Inferring Regulatory Programs Governing Region Specificity of Neuroepithelial Stem Cells during Early Hindbrain and Spinal Cord Development. Cell Syst, 9(2), 167-186 e112. https://doi.org/10.1016/j.cels.2019.05.012
Chisholm, A. E., Qaiser, T., Williams, A. M. M., Eginyan, G., & Lam, T. (2019). Acquisition of a precision walking skill and the impact of proprioceptive deficits in people with motor-incomplete spinal cord injury. J Neurophysiol, 121(3), 1078-1084. https://doi.org/10.1152/jn.00432.2018
Ditunno, J. F., Jr., Ditunno, P. L., Scivoletto, G., Patrick, M., Dijkers, M., Barbeau, H., Burns, A. S., Marino, R. J., & Schmidt-Read, M. (2013). The Walking Index for Spinal Cord Injury (WISCI/WISCI II): nature, metric properties, use and misuse. Spinal Cord, 51(5), 346-355. https://doi.org/10.1038/sc.2013.9
Gaspar, R., Padula, N., Freitas, T. B., de Oliveira, J. P. J., & Torriani-Pasin, C. (2019). Physical Exercise for Individuals With Spinal Cord Injury: Systematic Review Based on the International Classification of Functioning, Disability, and Health. J Sport Rehabil, 28(5), 505-516. https://doi.org/10.1123/jsr.2017-0185
Hicks, A. L. (2020). Locomotor training in people with spinal cord injury: is this exercise? Spinal Cord. https://doi.org/10.1038/s41393-020-0502-y
Hidalgo Martínez, Á. (2017). La rehabilitación terapéutica a pacientes parapléjicos: impacto desde las tecnologías. Podium. Revista de Ciencia y Tecnologia en la Cultura Física, 12(1), 21-30. http://podium.upr.edu.cu/index.php/podium/article/view/687
Holanda, L. J., Silva, P. M. M., Amorim, T. C., Lacerda, M. O., Simao, C. R., & Morya, E. (2017). Robotic assisted gait as a tool for rehabilitation of individuals with spinal cord injury: a systematic review. J Neuroeng Rehabil, 14(1), 126. https://doi.org/10.1186/s12984-017-0338-7
Hutson, T. H., & Di Giovanni, S. (2019). The translational landscape in spinal cord injury: focus on neuroplasticity and regeneration. Nat Rev Neurol, 15(12), 732-745. https://doi.org/10.1038/s41582-019-0280-3
Jiménez-Pascual, L. M. (2013). Concepción metodológica para el perfeccionamiento de la hidrocinesiterapia en el lesionado medular del Hospital "Julio Díaz" [Tesis Doctoral, Universidad de Ciencias de la Cultura Física y el Deporte "Manuel Fajardo"]. La Habana.
Mazzoleni, S., Battini, E., Rustici, A., & Stampacchia, G. (2017). An integrated gait rehabilitation training based on Functional Electrical Stimulation cycling and overground robotic exoskeleton in complete spinal cord injury patients: Preliminary results. IEEE Int Conf Rehabil Robot, 2017, 289-293. https://doi.org/10.1109/ICORR.2017.8009261
McDaid, D., Park, A. L., Gall, A., Purcell, M., & Bacon, M. (2019). Understanding and modelling the economic impact of spinal cord injuries in the United Kingdom. Spinal Cord, 57(9), 778-788. https://doi.org/10.1038/s41393-019-0285-1
Mekki, M., Delgado, A. D., Fry, A., Putrino, D., & Huang, V. (2018). Robotic Rehabilitation and Spinal Cord Injury: a Narrative Review. Neurotherapeutics, 15(3), 604-617. https://doi.org/10.1007/s13311-018-0642-3
Midik, M., Paker, N., Bugdayci, D., & Midik, A. C. (2020). Effects of robot-assisted gait training on lower extremity strength, functional independence, and walking function in men with incomplete traumatic spinal cord injury. Turk J Phys Med Rehabil, 66(1), 54-59. https://doi.org/10.5606/tftrd.2020.3316
Miller, L. E., Zimmermann, A. K., & Herbert, W. G. (2016). Clinical effectiveness and safety of powered exoskeleton-assisted walking in patients with spinal cord injury: systematic review with meta-analysis. Med Devices, 9, 455-466. https://pubmed.ncbi.nlm.nih.gov/27042146/
Mulcahey, M. J., Calhoun, C. L., Sinko, R., Kelly, E. H., & Vogel, L. C. (2016). The spinal cord independence measure (SCIM)-III self report for youth. Spinal Cord, 54(3), 204-212. https://doi.org/10.1038/sc.2015.103
Okawara, H., Sawada, T., Matsubayashi, K., Sugai, K., Tsuji, O., Nagoshi, N., Matsumoto, M., & Nakamura, M. (2020). Gait ability required to achieve therapeutic effect in gait and balance function with the voluntary driven exoskeleton in patients with chronic spinal cord injury: a clinical study. Spinal Cord, 58(5), 520-527. https://doi.org/10.1038/s41393-019-0403-0
Ribeiro Neto, F., Gomes Costa, R. R., Tanhoffer, R. A., Leal, J. C., Bottaro, M., & Carregaro, R. L. (2020). Muscle Strength Cutoff Points for Functional Independence and Wheelchair Ability in Men With Spinal Cord Injury. Arch Phys Med Rehabil, 101(6), 985-993. https://doi.org/10.1016/j.apmr.2020.01.010
Sandrow-Feinberg, H. R., & Houlé, J. D. J. B. r. (2015). Exercise after spinal cord injury as an agent for neuroprotection, regeneration and rehabilitation. 16-19, 12-21. https://pubmed.ncbi.nlm.nih.gov/25866284/
Silva, M. S., & Rodríguez, L. P. (2004). Ejercicios y metodología de enseñanza para la marcha en paraplejías con niveles de lesión media y baja D7-L2. Revista Digital - Buenos Aires 10(75) 19-25. https://www.efdeportes.com/efd75/lm.htm
Sutton, B. S., Ottomanelli, L., Njoh, E., Barnett, S., & Goetz, L. (2020). Economic evaluation of a supported employment program for veterans with spinal cord injury. Disabil Rehabil, 42(10), 1423-1429. https://doi.org/10.1080/09638288.2018.1527955
Conflict of interests:
The authors declare not to have any interest conflicts.
Authors' contribution:
Alexander Echemendia del Valle: Conception of the idea, literature search and review, instrument making, instrument application, compilation of information resulting from the instruments applied,
statistic análisis, preparation of tables, graphs, and images, database preparation,
general advice on the topic addressed, drafting of the original (first version),
review and final version of the article, article correction, authorship coordinator,
translation of terms or information obtained, review of the application of the applied bibliographic standard
![]()
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0
International license
Copyright (c) 2021 Alexander Echemendia del Valle